The process of obtaining prior authorization for medications can be a daunting task, especially when it comes to navigating the complexities of health insurance plans. Ambetter, a popular health insurance provider, has implemented a prior authorization process to ensure that patients receive the necessary medications while also managing healthcare costs. In this article, we will break down the Ambetter pharmacy prior authorization process into 5 easy steps, providing you with a comprehensive guide to help you navigate this process with ease.
What is Prior Authorization?
Prior authorization, also known as pre-authorization, is a process used by health insurance providers to determine whether a medication or treatment is medically necessary before approving coverage. This process helps to ensure that patients receive the most effective and cost-efficient treatment options while also managing healthcare costs.
Step 1: Determine if Prior Authorization is Required
Before starting the prior authorization process, it's essential to determine if prior authorization is required for the specific medication or treatment. You can check the Ambetter website or contact their customer service department to confirm whether prior authorization is necessary. Additionally, you can also consult with your healthcare provider or pharmacist to determine if prior authorization is required.

Step 2: Gather Required Information
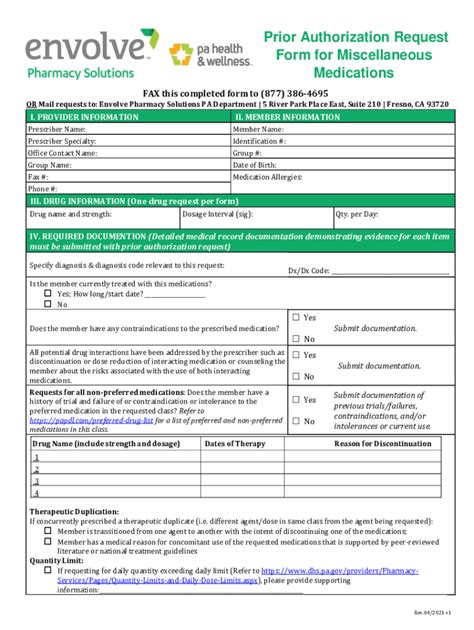
To initiate the prior authorization process, you'll need to gather the required information, which typically includes:
- Patient demographics (name, date of birth, etc.)
- Prescription information (medication name, dosage, frequency, etc.)
- Medical history and diagnosis
- Healthcare provider information (name, contact information, etc.)
- Insurance information (policy number, group number, etc.)
You can usually obtain this information from your healthcare provider or pharmacist.
Step 3: Submit the Prior Authorization Request
Once you've gathered the required information, you can submit the prior authorization request to Ambetter. You can do this through:
- Ambetter's online portal
- Faxing the request to Ambetter's prior authorization department
- Calling Ambetter's customer service department
Be sure to follow the specific instructions provided by Ambetter to ensure that your request is processed correctly.

Step 4: Wait for Approval or Denial
After submitting the prior authorization request, Ambetter will review the information and make a determination regarding coverage. This process typically takes a few days to a week, but may vary depending on the complexity of the request.
If approved, Ambetter will notify you and your healthcare provider, and you can proceed with filling the prescription. If denied, Ambetter will provide a reason for the denial and may offer alternative treatment options.
Step 5: Appeal the Decision (If Necessary)
If your prior authorization request is denied, you have the right to appeal the decision. To appeal, you'll need to provide additional information or documentation to support the medical necessity of the medication or treatment.
You can submit an appeal through:
- Ambetter's online portal
- Faxing the appeal to Ambetter's appeals department
- Calling Ambetter's customer service department
Be sure to follow the specific instructions provided by Ambetter to ensure that your appeal is processed correctly.

Tips and Reminders
- Always check the Ambetter website or contact their customer service department to confirm prior authorization requirements and procedures.
- Ensure that all required information is accurate and complete to avoid delays or denials.
- Keep a record of your prior authorization requests and appeals for future reference.
- Don't hesitate to reach out to your healthcare provider or pharmacist for assistance with the prior authorization process.
Common Questions and Concerns
- Q: How long does the prior authorization process take?
- A: The prior authorization process typically takes a few days to a week, but may vary depending on the complexity of the request.
- Q: What happens if my prior authorization request is denied?
- A: If your prior authorization request is denied, you have the right to appeal the decision. You can submit an appeal through Ambetter's online portal, fax, or phone.
- Q: Can I expedite the prior authorization process?
- A: Yes, Ambetter offers an expedited review process for urgent or emergency situations. Contact their customer service department for more information.
What is the purpose of prior authorization?
+Prior authorization is a process used by health insurance providers to determine whether a medication or treatment is medically necessary before approving coverage.
How do I know if prior authorization is required for my medication?
+You can check the Ambetter website or contact their customer service department to confirm whether prior authorization is necessary for your medication.
What happens if my prior authorization request is approved?
+If your prior authorization request is approved, Ambetter will notify you and your healthcare provider, and you can proceed with filling the prescription.
By following these 5 easy steps, you can navigate the Ambetter pharmacy prior authorization process with ease. Remember to stay informed, plan ahead, and don't hesitate to reach out to your healthcare provider or pharmacist for assistance.