Receiving quality medical care can be a complex and often frustrating process, especially when it comes to navigating the world of health insurance. One crucial aspect of this process is prior authorization, which can significantly impact the timely delivery of necessary treatments. For individuals covered by Ambetter, understanding the inpatient prior authorization process is essential to ensure seamless access to care. This article aims to provide a comprehensive, step-by-step guide to the Ambetter inpatient prior authorization form, aiming to demystify the process and equip readers with the knowledge they need to navigate it successfully.
The importance of prior authorization cannot be overstated. It serves as a critical mechanism for health insurance providers to ensure that the treatments and services covered are medically necessary and align with established standards of care. For patients, understanding and navigating this process can mean the difference between receiving timely care and facing delays or even denials of service.

Understanding the Basics of Ambetter Inpatient Prior Authorization
Before delving into the specifics of the Ambetter inpatient prior authorization form, it's essential to grasp the basics of what prior authorization entails and why it's necessary.
What is Prior Authorization?
Prior authorization is a process where a healthcare provider must obtain approval from a patient's health insurance provider before administering certain treatments, procedures, or prescribing specific medications. This process is designed to ensure that the treatments are medically necessary and fall within the scope of the patient's insurance coverage.
Why is Prior Authorization Necessary?
Prior authorization is necessary for several reasons, including ensuring that patients receive the most appropriate and cost-effective care. It helps in managing healthcare costs by preventing unnecessary treatments and promotes the use of evidence-based medicine.
A Step-by-Step Guide to the Ambetter Inpatient Prior Authorization Form
Navigating the Ambetter inpatient prior authorization process involves several steps, each crucial for ensuring that the authorization is processed efficiently.
Step 1: Determine if Prior Authorization is Required
Not all treatments or services require prior authorization. The first step involves determining whether the specific service or treatment your patient needs requires authorization. This information can usually be found in the Ambetter policy documents or by contacting Ambetter directly.
Step 2: Gather Necessary Information
Before starting the authorization process, gather all necessary information, including:
- Patient demographics
- Diagnosis and treatment details
- Medication lists
- Previous treatment records, if applicable
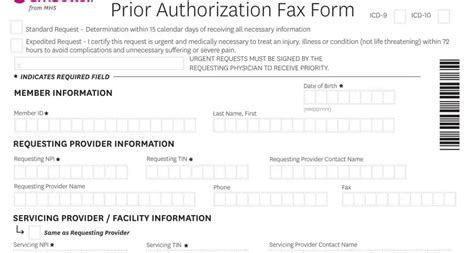
Step 3: Complete the Prior Authorization Form
Once you have all the necessary information, the next step is to complete the Ambetter inpatient prior authorization form. This form will require detailed information about the patient, the treatment or service being requested, and the clinical rationale for the request.

Step 4: Submit the Form
After completing the form, the next step is to submit it to Ambetter for review. This can usually be done electronically or by fax, depending on the instructions provided by Ambetter.
Step 5: Wait for the Authorization Decision
After submitting the form, wait for the authorization decision from Ambetter. This can take a few days to a week, depending on the complexity of the request and the workload of the authorization team.
Step 6: Receive and Review the Authorization Decision
Once the decision is made, Ambetter will notify you of the outcome. If approved, ensure you understand the scope of the authorization, including any limitations or conditions. If denied, you may have the option to appeal the decision.
Tips for Successfully Navigating the Ambetter Inpatient Prior Authorization Process
While the process can seem daunting, there are several strategies you can employ to ensure a smoother experience:
- Plan Ahead: Allow plenty of time for the authorization process to avoid last-minute rushes.
- Be Thorough: Ensure all information is accurate and complete to avoid delays.
- Stay Organized: Keep a record of all communications and submissions related to the authorization.
- Follow Up: If necessary, follow up with Ambetter to check on the status of your request.
Conclusion and Call to Action
Navigating the Ambetter inpatient prior authorization process requires patience, attention to detail, and a clear understanding of the steps involved. By following the guide outlined above and staying informed, you can better navigate this critical aspect of healthcare management. If you have any questions or need further clarification on any of the steps, we encourage you to comment below or reach out to Ambetter directly for support.
What is the purpose of prior authorization?
+Prior authorization is a process designed to ensure that treatments and services covered by insurance are medically necessary and align with established standards of care.
How long does the prior authorization process typically take?
+The duration can vary, but it usually takes a few days to a week for Ambetter to make an authorization decision.
What should I do if my prior authorization request is denied?
+If your request is denied, you may have the option to appeal the decision. Review the denial letter for specific instructions on how to proceed.