Streamlining Healthcare: The Importance of Easy Allwell Prior Authorization
Prior authorization is a critical step in the healthcare process, ensuring that patients receive the necessary treatments while also controlling healthcare costs. However, traditional prior authorization methods can be cumbersome, time-consuming, and even frustrating for healthcare providers and patients alike. This is where Easy Allwell prior authorization comes into play, simplifying the process and making it more efficient for all parties involved.
The Benefits of Easy Allwell Prior Authorization
Prior authorization is essential in preventing unnecessary medical procedures and reducing healthcare costs. By streamlining the prior authorization process, healthcare providers can focus on what matters most – providing high-quality patient care. Easy Allwell prior authorization offers several benefits, including:
- Reduced administrative burden: Automating the prior authorization process saves time and reduces the workload for healthcare providers.
- Improved patient satisfaction: Faster authorization decisions lead to quicker treatment initiation, resulting in better patient outcomes and higher satisfaction rates.
- Enhanced accuracy: Electronic prior authorization systems minimize errors and reduce the risk of denied claims.

How Easy Allwell Prior Authorization Works in 5 Simple Steps
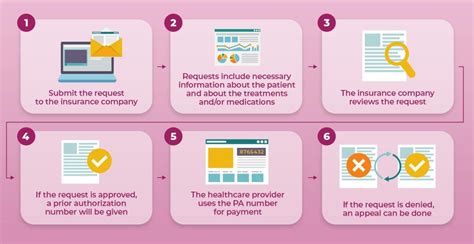
Easy Allwell prior authorization is designed to be user-friendly and efficient. Here's a step-by-step guide on how it works:
Step 1: Initial Request Submission
The healthcare provider submits a prior authorization request through the Easy Allwell online portal or via fax. The request includes patient demographics, diagnosis, treatment plan, and any relevant medical records.

Step 2: Automated Eligibility Verification
The Easy Allwell system automatically verifies the patient's eligibility and benefits, ensuring that the requested treatment is covered under their insurance plan.
Eligibility Verification Process
- Patient demographics verification
- Insurance coverage confirmation
- Benefits verification

Step 3: Clinical Review
A clinical reviewer assesses the prior authorization request to determine medical necessity. This step ensures that the requested treatment aligns with evidence-based guidelines and is necessary for the patient's condition.
Clinical Review Criteria
- Medical necessity evaluation
- Treatment plan review
- Patient medical history analysis

Step 4: Authorization Decision
The Easy Allwell system generates an authorization decision based on the clinical review. If approved, the healthcare provider receives an authorization number, which can be used to bill the insurance company.
Authorization Decision Options
- Approved with no additional requirements
- Approved with additional requirements (e.g., step therapy)
- Denied (with clear explanation and next steps)

Step 5: Ongoing Monitoring and Support
The Easy Allwell system provides ongoing monitoring and support to ensure that patients receive the necessary treatments and follow-up care. Healthcare providers can track patient progress, receive notifications, and access clinical resources through the online portal.
Ongoing Monitoring and Support Features
- Patient tracking and monitoring
- Clinical resource access
- Notification and alerts

Conclusion: Simplifying Healthcare with Easy Allwell Prior Authorization
Easy Allwell prior authorization streamlines the prior authorization process, reducing administrative burdens and improving patient satisfaction. By following the 5 simple steps outlined above, healthcare providers can efficiently navigate the prior authorization process, ensuring that patients receive the necessary treatments in a timely and cost-effective manner.
We invite you to share your thoughts and experiences with prior authorization in the comments below. How can we further simplify the process to improve patient care? Let's work together to create a more efficient and patient-centric healthcare system.
What is prior authorization, and why is it necessary?
+Prior authorization is a process that ensures patients receive necessary treatments while controlling healthcare costs. It involves verifying the medical necessity of a treatment plan before it is administered.
How does Easy Allwell prior authorization benefit healthcare providers?
+Easy Allwell prior authorization benefits healthcare providers by reducing administrative burdens, improving patient satisfaction, and enhancing accuracy. It also enables them to focus on providing high-quality patient care.
What is the typical turnaround time for prior authorization decisions with Easy Allwell?
+The typical turnaround time for prior authorization decisions with Easy Allwell is within 24-48 hours. However, this may vary depending on the complexity of the request and the availability of required documentation.