As a Medicare beneficiary, navigating the complex world of healthcare claims and appeals can be overwhelming. If your Medicare claim has been denied or partially denied, you may be wondering what steps to take next. One option is to file a reconsideration appeal, and that's where the Aetna Medicare Reconsideration Form comes in. In this article, we'll break down the process of completing and submitting this form, helping you to understand your rights and take control of your healthcare.
If you've received a denial or partial denial of your Medicare claim, it's essential to act quickly. Medicare has strict deadlines for filing appeals, and missing these deadlines can result in your claim being closed. By understanding the reconsideration process and using the Aetna Medicare Reconsideration Form, you can ensure that your appeal is processed efficiently and effectively.
Understanding the Medicare Appeals Process
Before we dive into the specifics of the Aetna Medicare Reconsideration Form, it's crucial to understand the Medicare appeals process. There are five levels of appeal, each with its own set of rules and deadlines.
- Redetermination: The first level of appeal, where you'll need to submit a written request to Medicare.
- Reconsideration: The second level of appeal, where a different Medicare representative will review your case.
- Hearing with an Administrative Law Judge (ALJ): The third level of appeal, where you'll have the opportunity to present your case to an ALJ.
- Review by the Medicare Appeals Council (MAC): The fourth level of appeal, where a council of experts will review your case.
- Federal District Court: The final level of appeal, where you can take your case to federal court.
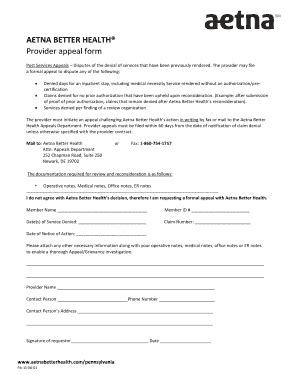
Completing the Aetna Medicare Reconsideration Form
The Aetna Medicare Reconsideration Form is a critical document that will help you to appeal a denial or partial denial of your Medicare claim. Here's a step-by-step guide to completing the form:

- Section 1: Beneficiary Information
- Enter your Medicare ID number and name.
- Provide your address, phone number, and email address.
- Section 2: Claim Information
- Enter the claim number and date of service.
- Describe the medical service or treatment in question.
- Section 3: Reason for Appeal
- Clearly state the reason for your appeal.
- Provide supporting documentation, such as medical records or test results.
- Section 4: Supporting Documentation
- Attach any additional documentation that supports your appeal.
- This may include letters from your doctor or medical records.
- Section 5: Signature
- Sign and date the form.
Tips for Submitting the Aetna Medicare Reconsideration Form
Once you've completed the form, it's essential to submit it correctly to ensure that your appeal is processed efficiently. Here are some tips to keep in mind:
- Submit the form within the deadline: Medicare has strict deadlines for filing appeals. Make sure to submit the form within 60 days of receiving the denial or partial denial letter.
- Use certified mail: Send the form via certified mail to ensure that it's received by Medicare.
- Keep a copy: Make a copy of the form and supporting documentation for your records.
What to Expect After Submitting the Aetna Medicare Reconsideration Form
After submitting the form, you can expect to receive a response from Medicare within 60 days. Here are some possible outcomes:
- Approved: Medicare may approve your appeal and pay for the medical service or treatment in question.
- Denied: Medicare may deny your appeal, in which case you can proceed to the next level of appeal.
- Partial Approval: Medicare may partially approve your appeal, paying for some but not all of the medical service or treatment in question.
Conclusion
Navigating the Medicare appeals process can be complex and time-consuming. By using the Aetna Medicare Reconsideration Form and following the steps outlined in this article, you can ensure that your appeal is processed efficiently and effectively. Remember to act quickly, as Medicare has strict deadlines for filing appeals. Don't hesitate to reach out to Medicare or a healthcare advocate if you need help with the process.
Additional Resources
- Medicare.gov:
- Aetna Medicare:
FAQ Section
What is the deadline for submitting the Aetna Medicare Reconsideration Form?
+The deadline for submitting the Aetna Medicare Reconsideration Form is 60 days from the date of the denial or partial denial letter.
Can I submit the Aetna Medicare Reconsideration Form online?
+No, the Aetna Medicare Reconsideration Form must be submitted via mail or fax.
How long does it take to receive a response from Medicare after submitting the Aetna Medicare Reconsideration Form?
+Medicare typically responds to appeals within 60 days of receiving the Aetna Medicare Reconsideration Form.