The Medicare Advantage program offers beneficiaries an alternative way to receive their Medicare benefits through private insurance companies, such as Aetna. While these plans can provide additional benefits and lower out-of-pocket costs, they can also lead to frustration and disappointment when claims are denied. If you're an Aetna Medicare Advantage plan holder and have received a denial of coverage, don't worry – you have the right to appeal the decision. In this article, we'll guide you through the 5 steps to file an Aetna Medicare Advantage appeal form.
Understanding the Appeal Process

Before we dive into the step-by-step guide, it's essential to understand the appeal process. The Medicare Advantage appeal process is designed to ensure that beneficiaries receive fair and timely decisions regarding their claims. If your claim is denied, you can appeal the decision, and the plan will review your case again. If the appeal is still denied, you can further appeal to an independent reviewer.
Why Appeal a Denied Claim?
Appealing a denied claim can be a lengthy process, but it's worth the effort. By appealing, you may be able to:
- Reverse the denial and receive coverage for the denied service or item
- Reduce your out-of-pocket costs
- Clarify any misunderstandings or miscommunications
- Ensure that your rights as a Medicare beneficiary are protected
Step 1: Review Your Denial Notice

The first step in appealing a denied claim is to carefully review your denial notice. This notice will explain the reason for the denial and provide instructions on how to appeal. Make sure to:
- Read the notice carefully and take note of the denial reason
- Check if the denial is due to a lack of information or documentation
- Verify the deadline for filing an appeal
What to Look for in the Denial Notice
When reviewing your denial notice, look for the following:
- The specific reason for the denial
- The plan's policy or guideline that supports the denial
- Any missing information or documentation required for coverage
- The deadline for filing an appeal
Step 2: Gather Supporting Documents

To build a strong appeal case, you'll need to gather supporting documents that demonstrate the medical necessity of the denied service or item. This may include:
- Medical records and test results
- Letters from your healthcare provider explaining the medical necessity of the service or item
- Documentation of any prior approvals or coverage for similar services or items
- Any relevant insurance policies or guidelines
What Documents to Include
When gathering supporting documents, include:
- Medical records from your healthcare provider
- Test results, lab reports, or imaging studies
- Letters from your healthcare provider explaining the medical necessity of the service or item
- Documentation of any prior approvals or coverage for similar services or items
Step 3: Complete the Aetna Medicare Advantage Appeal Form

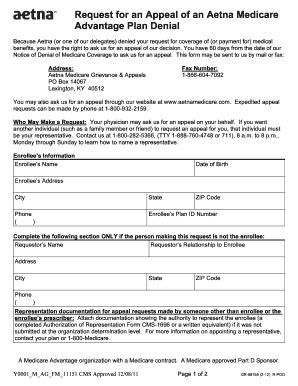
Once you've gathered supporting documents, it's time to complete the Aetna Medicare Advantage appeal form. You can obtain this form by:
- Visiting the Aetna website
- Contacting Aetna customer service
- Requesting the form from your healthcare provider
When completing the form, be sure to:
- Clearly explain the reason for the appeal
- Provide detailed information about the denied service or item
- Attach supporting documents and evidence
Tips for Completing the Appeal Form
When completing the appeal form, keep the following tips in mind:
- Be clear and concise in your explanation of the appeal
- Provide detailed information about the denied service or item
- Attach supporting documents and evidence
- Keep a copy of the completed form for your records
Step 4: Submit the Appeal Form

After completing the appeal form, submit it to Aetna along with any supporting documents and evidence. You can submit the form by:
- Mail: Send the form to the address listed on the denial notice
- Fax: Fax the form to the number listed on the denial notice
- Online: Upload the form to the Aetna website
Tracking Your Appeal
Once you've submitted the appeal form, be sure to:
- Track the status of your appeal
- Verify that Aetna received your appeal
- Follow up with Aetna if you haven't received a decision within the expected timeframe
Step 5: Follow Up on Your Appeal

After submitting your appeal, follow up with Aetna to ensure that your appeal is being processed. You can:
- Call Aetna customer service to check on the status of your appeal
- Check the Aetna website for updates on your appeal
- Send a follow-up letter or email to Aetna if you haven't received a decision within the expected timeframe
Next Steps After the Appeal Decision
If your appeal is approved, you'll receive coverage for the denied service or item. If your appeal is denied, you can further appeal to an independent reviewer. In either case, be sure to:
- Understand the decision and any next steps
- Follow the instructions provided by Aetna
- Seek assistance from a Medicare advocate or counselor if needed
By following these 5 steps, you can file an Aetna Medicare Advantage appeal form and advocate for your rights as a Medicare beneficiary.
What is the deadline for filing an Aetna Medicare Advantage appeal?
+The deadline for filing an Aetna Medicare Advantage appeal varies depending on the type of appeal. For a standard appeal, the deadline is 60 days from the date of the denial notice. For an expedited appeal, the deadline is 24 hours from the date of the denial notice.
Can I appeal an Aetna Medicare Advantage denial online?
+Yes, you can appeal an Aetna Medicare Advantage denial online through the Aetna website. You'll need to create an account and follow the online appeal process.
How long does it take to receive a decision on an Aetna Medicare Advantage appeal?
+The timeframe for receiving a decision on an Aetna Medicare Advantage appeal varies depending on the type of appeal. For a standard appeal, the decision is typically made within 30 days. For an expedited appeal, the decision is typically made within 24 hours.