Aetna Eylea prior authorization can be a time-consuming and frustrating process for healthcare providers and patients alike. However, with a clear understanding of the requirements and a streamlined approach, you can reduce the administrative burden and ensure timely access to this essential medication. In this article, we will break down the Aetna Eylea prior authorization process into 5 easy steps.
The Importance of Prior Authorization
Prior authorization is a critical step in ensuring that patients receive the necessary treatment while also managing healthcare costs. Aetna, like other insurance providers, requires prior authorization for certain medications, including Eylea, to ensure that they are prescribed and used judiciously. Eylea is a medication used to treat various eye conditions, including age-related macular degeneration, diabetic macular edema, and retinal vein occlusion.
Step 1: Verify Patient Eligibility and Benefits
Before initiating the prior authorization process, it is essential to verify the patient's eligibility and benefits. You can do this by:
- Contacting Aetna's customer service department
- Checking the patient's insurance card or policy documents
- Using Aetna's online portal or mobile app

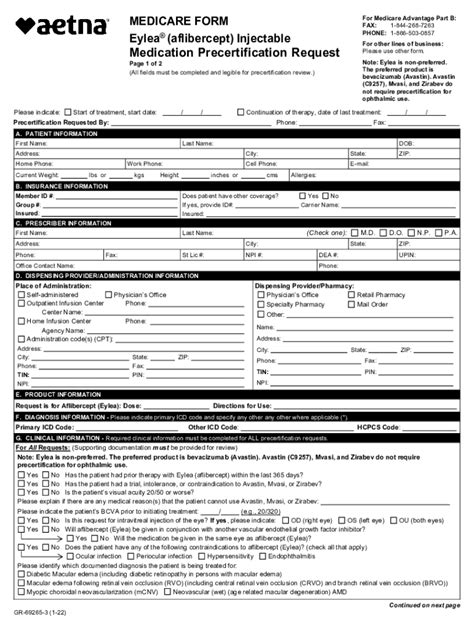
Step 2: Gather Required Documentation
To initiate the prior authorization process, you will need to gather the required documentation, including:
- Patient demographics and insurance information
- Medical records, including diagnosis and treatment history
- Prescription information, including dosage and frequency
- Laboratory results, including vision tests and imaging studies
Required Documentation Checklist:
- Patient demographics and insurance information
- Medical records, including diagnosis and treatment history
- Prescription information, including dosage and frequency
- Laboratory results, including vision tests and imaging studies
Step 3: Submit Prior Authorization Request
Once you have gathered the required documentation, you can submit the prior authorization request to Aetna. You can do this by:
- Faxing the request to Aetna's prior authorization department
- Submitting the request online through Aetna's portal or mobile app
- Mailing the request to Aetna's prior authorization department

Step 4: Respond to Additional Requests
Aetna may request additional information or documentation to support the prior authorization request. It is essential to respond promptly to these requests to avoid delays in the process.
Common Additional Requests:
- Additional medical records or laboratory results
- Clarification on prescription information or dosage
- Information on previous treatments or therapies
Step 5: Receive Prior Authorization Determination
Once Aetna has received all required documentation and information, they will review the prior authorization request and make a determination. You can expect to receive a decision within 3-5 business days.

Streamlining the Prior Authorization Process
By following these 5 easy steps, you can streamline the Aetna Eylea prior authorization process and reduce the administrative burden. Additionally, consider implementing the following strategies to further streamline the process:
- Use electronic prior authorization requests and submissions
- Designate a staff member to handle prior authorization requests
- Develop a checklist or template to ensure all required documentation is included
Invitation to Comment and Share
We hope this article has provided valuable insights into the Aetna Eylea prior authorization process. If you have any questions or comments, please feel free to share them below. Additionally, if you have experience with the prior authorization process, we invite you to share your tips and strategies for streamlining the process.
What is the average time frame for receiving a prior authorization determination from Aetna?
+Aetna typically makes a prior authorization determination within 3-5 business days.
Can I submit a prior authorization request online?
+Yes, Aetna offers an online portal and mobile app for submitting prior authorization requests.
What documentation is required for an Eylea prior authorization request?
+The required documentation includes patient demographics and insurance information, medical records, prescription information, and laboratory results.