Prior authorization is a crucial step in the healthcare process, ensuring that patients receive necessary treatments while controlling healthcare costs. For healthcare providers and patients alike, navigating the prior authorization process can be daunting, especially when dealing with specific forms like the Aetna Better Health Prior Authorization Form. In this article, we'll delve into the world of prior authorization, focusing on the Aetna Better Health Prior Authorization Form, to provide a comprehensive guide that simplifies the process.
Healthcare providers and patients often view prior authorization as a necessary evil, but it's essential to understand its importance. Prior authorization helps ensure that the prescribed treatment is medically necessary, reducing unnecessary healthcare costs. By approving treatments before they're administered, insurance providers can also guarantee that patients receive the most effective and safest care available.

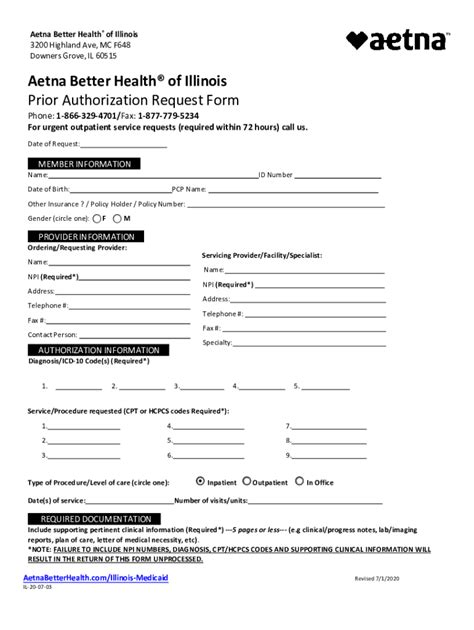
Aetna Better Health Prior Authorization Form: An Overview
Aetna Better Health is a leading health insurance provider that offers a range of plans, including Medicaid and Medicare Advantage. The Aetna Better Health Prior Authorization Form is a critical document that healthcare providers must complete to request prior authorization for treatments, services, or medications.
Why is Prior Authorization Necessary?
Prior authorization is essential to ensure that patients receive the most effective and safe treatments while controlling healthcare costs. Here are some reasons why prior authorization is necessary:
- Ensures medically necessary treatments: Prior authorization guarantees that the prescribed treatment is medically necessary and aligns with the patient's health needs.
- Reduces unnecessary costs: By approving treatments before they're administered, insurance providers can reduce unnecessary healthcare costs.
- Improves patient safety: Prior authorization helps ensure that patients receive the safest and most effective treatments available.
How to Complete the Aetna Better Health Prior Authorization Form
Completing the Aetna Better Health Prior Authorization Form can be a daunting task, but breaking it down into smaller steps makes it more manageable. Here's a step-by-step guide to help you complete the form:
- Gather required information: Before starting the form, gather all necessary information, including the patient's demographic data, medical history, and treatment details.
- Choose the correct form: Ensure you're using the correct prior authorization form for Aetna Better Health.
- Fill out the form accurately: Complete the form accurately and thoroughly, providing all required information.
- Attach supporting documents: Attach all supporting documents, including medical records and test results.
- Submit the form: Submit the completed form to Aetna Better Health for review.

Aetna Better Health Prior Authorization Form Requirements
The Aetna Better Health Prior Authorization Form has specific requirements that must be met to ensure a smooth review process. Here are some key requirements:
- Patient information: Provide accurate and complete patient demographic data, including name, date of birth, and insurance information.
- Treatment details: Provide detailed information about the treatment, including the type of treatment, dosage, and duration.
- Medical history: Provide a detailed medical history, including relevant test results and medical records.
- Supporting documents: Attach all supporting documents, including medical records and test results.
Aetna Better Health Prior Authorization Form FAQ
Here are some frequently asked questions about the Aetna Better Health Prior Authorization Form:
Q: What is the Aetna Better Health Prior Authorization Form used for?
A: The Aetna Better Health Prior Authorization Form is used to request prior authorization for treatments, services, or medications.
Q: How long does the prior authorization process take?
A: The prior authorization process typically takes 2-5 business days, but may vary depending on the complexity of the request.
Q: What happens if my prior authorization request is denied?
A: If your prior authorization request is denied, you may appeal the decision by submitting additional information or supporting documents.
Conclusion
The Aetna Better Health Prior Authorization Form is a critical document that healthcare providers must complete to request prior authorization for treatments, services, or medications. By understanding the importance of prior authorization and following the steps outlined in this guide, healthcare providers can navigate the prior authorization process with ease.

If you have any questions or need further assistance with the Aetna Better Health Prior Authorization Form, please don't hesitate to comment below. Share this article with your colleagues and peers to help them navigate the prior authorization process.
What is the purpose of the Aetna Better Health Prior Authorization Form?
+The Aetna Better Health Prior Authorization Form is used to request prior authorization for treatments, services, or medications.
How long does the prior authorization process take?
+The prior authorization process typically takes 2-5 business days, but may vary depending on the complexity of the request.
What happens if my prior authorization request is denied?
+If your prior authorization request is denied, you may appeal the decision by submitting additional information or supporting documents.