As a healthcare provider, navigating the complexities of insurance claims and appeals can be a daunting task. One of the most critical aspects of this process is submitting a well-crafted appeal form to dispute denied claims or unfavorable reimbursement decisions. In this article, we will delve into the world of Wellmed provider appeal form submission, providing you with a comprehensive guide to help you effectively appeal denied claims and secure the reimbursement you deserve.
Understanding the Importance of Accurate Claim Submission
Before we dive into the specifics of the Wellmed provider appeal form, it's essential to understand the significance of accurate claim submission. When you submit a claim, it's crucial to ensure that all the required information is included, and the claim is filed correctly. Any errors or omissions can lead to delays, denials, or underpayment, resulting in lost revenue for your practice.

The Wellmed Provider Appeal Form: An Overview
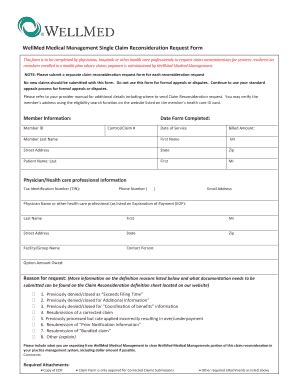
The Wellmed provider appeal form is a critical document that allows you to dispute denied claims or unfavorable reimbursement decisions. The form is designed to provide a structured format for submitting appeals, ensuring that all necessary information is included.
Key Components of the Wellmed Provider Appeal Form
The Wellmed provider appeal form typically consists of several key components, including:
- Patient Information: This section requires you to provide detailed information about the patient, including their name, date of birth, and policy number.
- Claim Information: In this section, you'll need to provide details about the claim, including the claim number, date of service, and procedure codes.
- Reason for Appeal: This is the most critical section of the form, where you'll need to clearly explain why you're appealing the denied claim or reimbursement decision.
- Supporting Documentation: You'll need to attach supporting documentation, such as medical records, test results, and treatment plans, to substantiate your appeal.

Tips for Submitting a Successful Wellmed Provider Appeal Form
To increase your chances of a successful appeal, follow these tips when submitting your Wellmed provider appeal form:
- Ensure Accuracy: Double-check all the information on the form, including patient details, claim numbers, and procedure codes.
- Clearly Explain the Reason for Appeal: Use clear and concise language to explain why you're appealing the denied claim or reimbursement decision.
- Attach Supporting Documentation: Make sure to attach all relevant supporting documentation, including medical records and test results.
- Meet the Deadline: Submit your appeal form within the specified timeframe to avoid missing the deadline.

Common Mistakes to Avoid When Submitting a Wellmed Provider Appeal Form
When submitting a Wellmed provider appeal form, there are several common mistakes to avoid, including:
- Incomplete Information: Failing to provide all the required information can lead to delays or denials.
- Inaccurate Information: Providing inaccurate information can result in denials or underpayment.
- Missing Deadlines: Failing to submit the appeal form within the specified timeframe can result in missed opportunities for reimbursement.

The Appeals Process: What to Expect
Once you've submitted your Wellmed provider appeal form, the appeals process will begin. Here's what you can expect:
- Initial Review: The appeal will be reviewed by a representative from Wellmed to determine whether the appeal meets the necessary criteria.
- Additional Information: You may be requested to provide additional information or supporting documentation to support your appeal.
- Decision: A decision will be made regarding your appeal, which may include approval, denial, or partial approval.

Conclusion
Submitting a Wellmed provider appeal form requires attention to detail, accuracy, and a clear understanding of the appeals process. By following the tips and guidelines outlined in this article, you can increase your chances of a successful appeal and secure the reimbursement you deserve. Remember to avoid common mistakes, ensure accuracy, and provide supporting documentation to support your appeal.
Take Action
Now that you've read this comprehensive guide to submitting a Wellmed provider appeal form, take action by:
- Reviewing your current appeal process to identify areas for improvement
- Updating your appeal form template to ensure accuracy and completeness
- Providing training to your staff on the appeals process and best practices
By taking these steps, you can optimize your appeal process, reduce denials, and increase reimbursement.
FAQs
What is the deadline for submitting a Wellmed provider appeal form?
+The deadline for submitting a Wellmed provider appeal form varies depending on the specific plan and policy. It's essential to check the plan documents or contact Wellmed directly to determine the deadline.
What information do I need to provide on the Wellmed provider appeal form?
+You'll need to provide detailed information about the patient, claim, and reason for appeal, as well as attach supporting documentation, such as medical records and test results.
How long does the appeals process take?
+The length of time for the appeals process varies depending on the complexity of the appeal and the volume of appeals being processed. You can expect a decision within 30-60 days, but this timeframe may be longer in some cases.