Prior authorization is a crucial step in the healthcare process, ensuring that patients receive the necessary medical treatment while also controlling healthcare costs. WellMed, a leading healthcare provider, has implemented a prior authorization process to streamline the approval of medical treatments. In this article, we will guide you through the 5 easy steps to complete a WellMed prior authorization form.

Understanding the Importance of Prior Authorization
Prior authorization is a process used by healthcare providers to determine whether a specific medical treatment or service is medically necessary. This process helps ensure that patients receive the most effective and cost-efficient care possible. By completing a prior authorization form, healthcare providers can verify that the proposed treatment aligns with the patient's medical needs and the insurance coverage.
Benefits of Prior Authorization
Prior authorization offers several benefits to both patients and healthcare providers. Some of the key advantages include:
- Ensuring that patients receive medically necessary treatment
- Reducing healthcare costs by avoiding unnecessary treatments
- Streamlining the approval process for medical treatments
- Improving patient outcomes by ensuring timely access to necessary care
Step 1: Gather Required Information
Before starting the prior authorization process, it is essential to gather all the necessary information. This includes:
- Patient's demographic information (name, date of birth, etc.)
- Patient's medical history and current diagnosis
- Proposed treatment or service information (including CPT codes and ICD-10 codes)
- Insurance information (policy number, coverage details, etc.)

Required Documents
To complete the prior authorization form, you may need to provide additional documents, such as:
- Medical records and test results
- Prescription information
- Treatment plans and progress notes
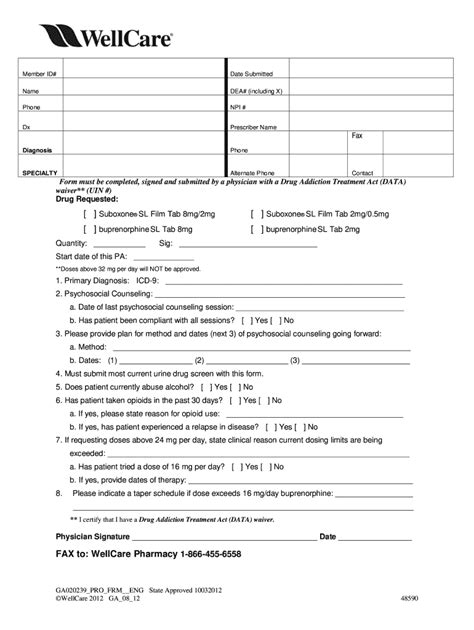
Step 2: Complete the Prior Authorization Form
Once you have gathered all the necessary information, you can start completing the prior authorization form. The form typically includes sections for:
- Patient information
- Treatment information
- Medical justification
- Insurance information

Tips for Completing the Form
When completing the prior authorization form, keep the following tips in mind:
- Ensure all sections are complete and accurate
- Use clear and concise language when explaining the medical justification
- Provide all required documents and supporting information
Step 3: Submit the Prior Authorization Form
After completing the prior authorization form, you can submit it to WellMed for review. You can submit the form via:
- Fax: [insert fax number]
- Mail: [insert mailing address]
- Online portal: [insert online portal link]

Submission Timeline
It is essential to submit the prior authorization form in a timely manner to avoid delays in the approval process. WellMed typically reviews prior authorization requests within [insert timeframe].
Step 4: Review and Follow-up
After submitting the prior authorization form, it is crucial to review the status of your request and follow up as necessary. You can:
- Check the status of your request online or via phone
- Follow up with WellMed to ensure timely processing
- Provide additional information or clarification as requested

Common Reasons for Denial
If your prior authorization request is denied, it may be due to:
- Insufficient medical justification
- Lack of required documentation
- Non-compliance with WellMed's coverage policies
Step 5: Appeal the Decision (If Necessary)
If your prior authorization request is denied, you can appeal the decision. To appeal, you will need to:
- Review the denial letter and understand the reason for denial
- Gather additional information or documentation to support your appeal
- Submit the appeal request to WellMed within the specified timeframe

Appeal Timeline
WellMed typically reviews appeal requests within [insert timeframe]. It is essential to submit the appeal request in a timely manner to avoid delays in the approval process.
By following these 5 easy steps, you can successfully complete a WellMed prior authorization form and ensure that your patients receive the necessary medical treatment. Remember to gather all required information, complete the form accurately, submit it in a timely manner, review and follow up, and appeal the decision if necessary.
What is prior authorization?
+Prior authorization is a process used by healthcare providers to determine whether a specific medical treatment or service is medically necessary.
Why is prior authorization necessary?
+Prior authorization ensures that patients receive medically necessary treatment, reduces healthcare costs, and streamlines the approval process for medical treatments.
How long does the prior authorization process take?
+WellMed typically reviews prior authorization requests within [insert timeframe].