Wellcare by Allwell authorization can be a complex and time-consuming process for healthcare providers. However, there are several ways to simplify this process, reducing administrative burdens and allowing providers to focus on what matters most – delivering high-quality patient care.
Understanding the Wellcare by Allwell Authorization Process

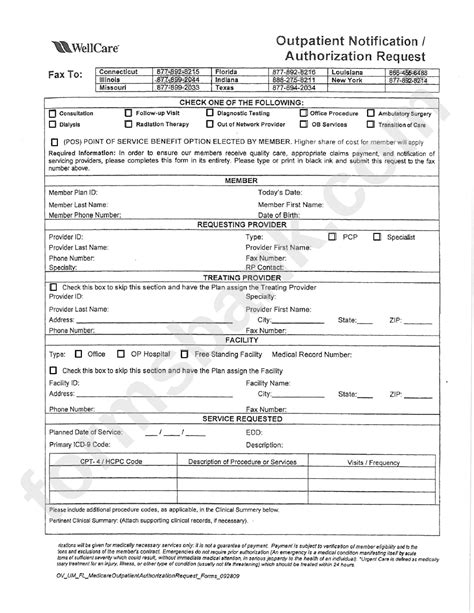
Before diving into the ways to simplify Wellcare by Allwell authorization, it's essential to understand the process itself. Wellcare by Allwell is a Medicare Advantage plan that requires prior authorization for certain medical services and prescription medications. The authorization process involves submitting requests to Wellcare by Allwell, which then reviews the requests to determine whether the requested services or medications are medically necessary.
1. Utilize Electronic Prior Authorization (ePA) Solutions

One way to simplify Wellcare by Allwell authorization is to utilize electronic prior authorization (ePA) solutions. ePA solutions allow healthcare providers to submit authorization requests electronically, reducing paperwork and streamlining the process. Many ePA solutions also offer real-time status updates and automatic notifications, making it easier to track the progress of authorization requests.
Benefits of ePA Solutions
• Reduced administrative burdens • Faster authorization decisions • Improved communication between providers and payers • Enhanced patient care through quicker access to necessary treatments
2. Leverage Wellcare by Allwell's Online Portal

Wellcare by Allwell offers an online portal that allows healthcare providers to submit authorization requests, check status updates, and access prior authorization guidelines. Leveraging this portal can simplify the authorization process by providing a centralized location for all prior authorization activities.
Benefits of Wellcare by Allwell's Online Portal
• Convenient access to prior authorization information • Streamlined submission process • Real-time status updates • Access to prior authorization guidelines and requirements
3. Implement a Prior Authorization Workflow

Implementing a prior authorization workflow can help simplify the Wellcare by Allwell authorization process by establishing clear procedures and protocols for submitting and tracking authorization requests. This can include designating a specific staff member or team to handle prior authorization requests, setting up a tracking system to monitor the progress of requests, and establishing communication protocols with Wellcare by Allwell.
Benefits of a Prior Authorization Workflow
• Improved efficiency and productivity • Reduced administrative burdens • Enhanced communication and collaboration between staff members • Better tracking and management of authorization requests
4. Educate Staff on Prior Authorization Requirements

Educating staff on prior authorization requirements is essential to simplifying the Wellcare by Allwell authorization process. This can include providing training on Wellcare by Allwell's prior authorization guidelines, requirements, and procedures, as well as ensuring that staff members understand the importance of accurate and complete documentation.
Benefits of Staff Education
• Improved understanding of prior authorization requirements • Reduced errors and rejections • Enhanced patient care through quicker access to necessary treatments • Increased staff confidence and productivity
5. Consider Outsourcing Prior Authorization

Finally, consider outsourcing prior authorization to a third-party vendor or service provider. This can help simplify the Wellcare by Allwell authorization process by transferring the administrative burdens to a specialized company or team.
Benefits of Outsourcing Prior Authorization
• Reduced administrative burdens • Improved efficiency and productivity • Enhanced patient care through quicker access to necessary treatments • Access to specialized expertise and knowledge
By implementing these strategies, healthcare providers can simplify the Wellcare by Allwell authorization process, reducing administrative burdens and improving patient care.
What is Wellcare by Allwell authorization?
+Wellcare by Allwell authorization is a process that requires healthcare providers to submit prior authorization requests for certain medical services and prescription medications.
What is the benefit of using ePA solutions?
+The benefit of using ePA solutions is that they allow healthcare providers to submit authorization requests electronically, reducing paperwork and streamlining the process.
How can I simplify the Wellcare by Allwell authorization process?
+You can simplify the Wellcare by Allwell authorization process by utilizing ePA solutions, leveraging Wellcare by Allwell's online portal, implementing a prior authorization workflow, educating staff on prior authorization requirements, and considering outsourcing prior authorization.
We hope this article has provided valuable insights into simplifying the Wellcare by Allwell authorization process. If you have any questions or comments, please feel free to share them below.