The healthcare system can be overwhelming, especially when it comes to navigating insurance coverage and pre-authorization requirements. If you're a healthcare provider or patient dealing with UPMC Health Plan, you know how crucial prior authorization (prior auth) is for ensuring smooth and efficient care. In this article, we'll break down the prior auth process into 5 easy steps, helping you understand what's required and how to streamline the process.

What is Prior Authorization?
Prior authorization, also known as pre-authorization or pre-certification, is a process where healthcare providers obtain approval from insurance companies before providing certain medical services or treatments. This ensures that the services are medically necessary and covered under the patient's insurance plan. In the case of UPMC Health Plan, prior auth is required for many services, including surgeries, hospital stays, and specialized treatments.
Step 1: Determine if Prior Auth is Required
The first step in the prior auth process is to determine if prior auth is required for the specific service or treatment. UPMC Health Plan provides a list of services that require prior auth on their website. You can also contact their customer service department to confirm whether prior auth is needed.

Step 2: Gather Required Information
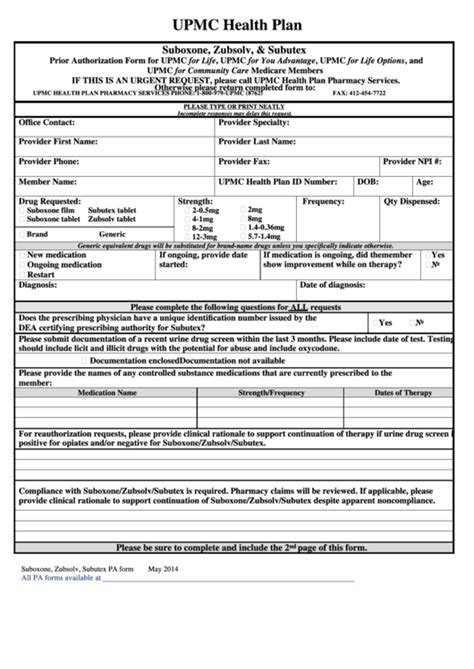
Once you've determined that prior auth is required, you'll need to gather the necessary information to submit a request. This typically includes:
- Patient demographic information
- Medical record numbers
- Service or treatment codes (e.g., CPT, ICD-10)
- Date of service
- Ordering physician's name and NPI
Make sure to have all the required information readily available to avoid delays in the prior auth process.
Step 3: Submit the Prior Auth Request
With all the necessary information gathered, you can submit the prior auth request to UPMC Health Plan. You can do this through their online portal, by phone, or by fax. Be sure to follow the specific submission guidelines provided by UPMC Health Plan to ensure timely processing.

Step 4: Receive and Review the Prior Auth Decision
After submitting the prior auth request, UPMC Health Plan will review the information and make a determination. You'll receive a notification with the decision, which may include:
- Approval: The service or treatment is approved, and you can proceed with scheduling.
- Denial: The service or treatment is not approved, and you may need to appeal the decision or explore alternative options.
- Additional Information Required: UPMC Health Plan may request additional information to make a determination.
Be sure to carefully review the decision and take any necessary next steps.
Step 5: Follow Up and Appeal (if necessary)
If your prior auth request is denied or you need to provide additional information, be sure to follow up with UPMC Health Plan in a timely manner. If you disagree with the decision, you may need to appeal. UPMC Health Plan provides an appeals process, which includes:
- Standard appeal: A review of the decision by a different UPMC Health Plan representative.
- Expedited appeal: A faster review process for urgent situations.

By following these 5 easy steps, you can navigate the UPMC Health Plan prior auth process with confidence. Remember to stay organized, gather all required information, and follow up as needed to ensure smooth and efficient care.

We hope this article has been informative and helpful in understanding the UPMC Health Plan prior auth process. If you have any further questions or concerns, please don't hesitate to reach out.
Conclusion
Navigating the prior auth process can be complex, but by breaking it down into manageable steps, you can ensure smooth and efficient care for your patients. Remember to stay informed, organized, and proactive throughout the process.

By following these 5 easy steps, you can streamline the UPMC Health Plan prior auth process and focus on what matters most – providing high-quality patient care.
Share Your Thoughts
Have you had any experiences with the UPMC Health Plan prior auth process? Share your thoughts and feedback in the comments below. Your insights can help others navigate the process and improve the overall quality of care.

FAQ Section:
What is the purpose of prior authorization?
+Prior authorization is a process where healthcare providers obtain approval from insurance companies before providing certain medical services or treatments.
How do I determine if prior auth is required for a specific service?
+You can check the UPMC Health Plan website or contact their customer service department to confirm whether prior auth is required.
What information do I need to submit a prior auth request?
+You'll need to gather patient demographic information, medical record numbers, service or treatment codes, date of service, and ordering physician's name and NPI.