The BCBS tier exception form is a crucial document for individuals who require medications that are not covered by their Blue Cross Blue Shield (BCBS) insurance plan. If you're facing a situation where your prescribed medication is not covered, understanding the tier exception process can help you navigate the system and potentially gain access to the medication you need. In this article, we'll delve into the key things you should know about the BCBS tier exception form.
When a medication is not covered by your insurance plan, it can be a significant concern, especially if you rely on that medication to manage a chronic condition. The tier exception process is designed to provide an avenue for individuals to request coverage for non-covered medications. This process can be complex, but with the right information, you can better understand what to expect.
Let's dive into the 5 key things you should know about the BCBS tier exception form.
What is the BCBS Tier Exception Form?

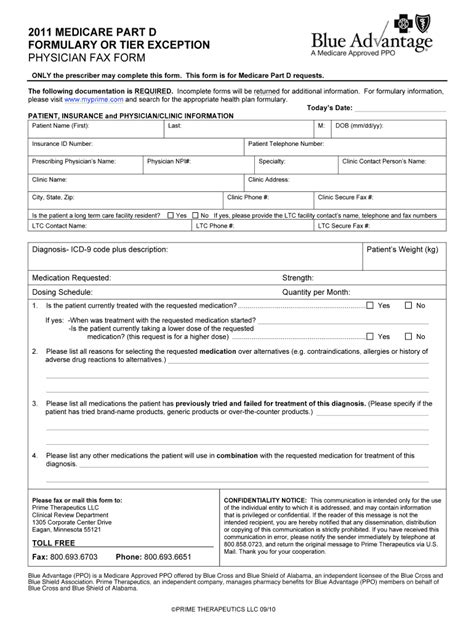
The BCBS tier exception form is a document that allows individuals to request an exception to their insurance plan's coverage rules. This form is typically used when a medication is not covered by the plan, but the individual's healthcare provider believes it is medically necessary. The form requires information from both the individual and their healthcare provider, and it must be submitted to BCBS for review.
Why is the BCBS Tier Exception Form Necessary?
The BCBS tier exception form is necessary because insurance plans often have specific rules and guidelines that determine which medications are covered. These rules can be based on a variety of factors, including the medication's efficacy, safety, and cost-effectiveness. When a medication is not covered, the tier exception form provides a way for individuals to request an exception to these rules.
How to Complete the BCBS Tier Exception Form

Completing the BCBS tier exception form requires careful attention to detail. Here are the steps to follow:
- Gather required information: Before starting the form, make sure you have all the necessary information, including your BCBS member ID, the name of the medication, and the reason why the medication is medically necessary.
- Fill out the form: The form typically requires information from both the individual and their healthcare provider. Make sure to fill out all required fields accurately and completely.
- Attach supporting documentation: You may need to attach supporting documentation, such as medical records or letters from your healthcare provider, to support your request.
- Submit the form: Once the form is complete, submit it to BCBS for review.
What Happens After Submitting the BCBS Tier Exception Form?
After submitting the BCBS tier exception form, BCBS will review your request to determine whether an exception can be made. This review process can take several days to several weeks, depending on the complexity of the request. If your request is approved, BCBS will notify you and your healthcare provider, and you will be able to access the medication. If your request is denied, you may be able to appeal the decision.
Common Reasons for BCBS Tier Exception Form Denials

While the BCBS tier exception form can be a valuable tool for gaining access to non-covered medications, there are several common reasons why requests may be denied. Here are a few:
- Lack of medical necessity: If BCBS determines that the medication is not medically necessary, the request may be denied.
- Insufficient documentation: If the supporting documentation is incomplete or insufficient, the request may be denied.
- Alternative treatments available: If alternative treatments are available that are covered by the plan, the request may be denied.
What to Do if Your BCBS Tier Exception Form is Denied
If your BCBS tier exception form is denied, there are several steps you can take. Here are a few:
- Appeal the decision: You may be able to appeal the decision by submitting additional information or documentation.
- Consult with your healthcare provider: Your healthcare provider may be able to provide additional guidance or support.
- Explore alternative treatments: If alternative treatments are available, you may be able to access them through your insurance plan.
Conclusion

The BCBS tier exception form can be a valuable tool for individuals who require medications that are not covered by their insurance plan. By understanding the key things to know about the form, including how to complete it and what happens after submitting it, you can better navigate the system and potentially gain access to the medication you need.
We hope this article has provided you with helpful information about the BCBS tier exception form. If you have any further questions or concerns, please don't hesitate to reach out. Share your thoughts and experiences in the comments below!
What is the BCBS tier exception form?
+The BCBS tier exception form is a document that allows individuals to request an exception to their insurance plan's coverage rules.
How do I complete the BCBS tier exception form?
+To complete the form, gather required information, fill out the form accurately and completely, attach supporting documentation, and submit the form to BCBS for review.
What happens after submitting the BCBS tier exception form?
+After submitting the form, BCBS will review your request to determine whether an exception can be made. If approved, BCBS will notify you and your healthcare provider, and you will be able to access the medication.