The Texas Standard Prior Authorization Form is a crucial document in the healthcare industry, particularly for healthcare providers and patients in Texas. Prior authorization, also known as pre-authorization or pre-certification, is a process used by health insurance companies to determine whether a patient's treatment or medication is medically necessary and covered under their policy. The Texas Standard Prior Authorization Form is designed to streamline this process, making it easier for healthcare providers to request prior authorization and for insurance companies to review and approve or deny these requests.
In this article, we will delve into the world of prior authorization, exploring the importance of the Texas Standard Prior Authorization Form, its benefits, and how it works. We will also provide guidance on how to fill out the form and what to expect during the prior authorization process.
What is Prior Authorization?

Prior authorization is a process used by health insurance companies to review and approve or deny medical treatments or medications before they are administered to a patient. This process is designed to ensure that patients receive necessary and effective care while also controlling healthcare costs. Prior authorization is typically required for certain treatments or medications, such as expensive or experimental procedures, or for patients with complex medical conditions.
Why is Prior Authorization Important?
Prior authorization is essential for several reasons:
- It helps to ensure that patients receive medically necessary care.
- It reduces the risk of adverse reactions or complications from unnecessary treatments.
- It controls healthcare costs by preventing unnecessary procedures or medication use.
- It improves patient safety by reducing the risk of medication errors or interactions.
What is the Texas Standard Prior Authorization Form?

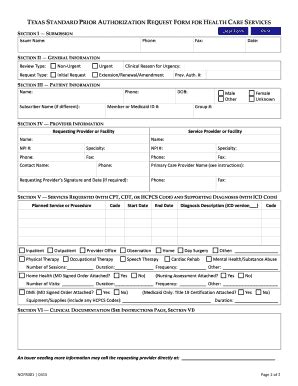
The Texas Standard Prior Authorization Form is a standardized form used by healthcare providers in Texas to request prior authorization from insurance companies. The form is designed to streamline the prior authorization process, making it easier for healthcare providers to request approval and for insurance companies to review and make decisions.
Benefits of the Texas Standard Prior Authorization Form
The Texas Standard Prior Authorization Form offers several benefits, including:
- Simplified prior authorization process
- Reduced administrative burden on healthcare providers
- Improved communication between healthcare providers and insurance companies
- Faster review and approval times
- Enhanced patient care and safety
How to Fill Out the Texas Standard Prior Authorization Form

Filling out the Texas Standard Prior Authorization Form requires careful attention to detail. Here are the steps to follow:
- Complete the patient information section: Include the patient's name, date of birth, and insurance information.
- Specify the treatment or medication: Clearly indicate the treatment or medication being requested, including the dosage and frequency.
- Provide medical justification: Explain why the treatment or medication is medically necessary, including any relevant medical history or test results.
- Attach supporting documentation: Include any relevant medical records, test results, or other supporting documentation.
- Sign and date the form: The healthcare provider must sign and date the form to certify that the information is accurate and complete.
What to Expect During the Prior Authorization Process

Once the Texas Standard Prior Authorization Form is submitted, the insurance company will review the request and make a determination. Here's what to expect:
- Review and approval: The insurance company will review the request and approve or deny it based on their policies and procedures.
- Notification: The healthcare provider and patient will be notified of the decision, usually within a few days.
- Appeals process: If the request is denied, the healthcare provider or patient can appeal the decision.
Conclusion
The Texas Standard Prior Authorization Form is a valuable tool for healthcare providers and patients in Texas. By streamlining the prior authorization process, it helps to ensure that patients receive necessary and effective care while also controlling healthcare costs. By following the steps outlined in this article, healthcare providers can fill out the form accurately and efficiently, and patients can receive the care they need.
What is prior authorization?
+Prior authorization is a process used by health insurance companies to review and approve or deny medical treatments or medications before they are administered to a patient.
Why is prior authorization important?
+Prior authorization is essential for several reasons, including ensuring that patients receive medically necessary care, reducing the risk of adverse reactions or complications, controlling healthcare costs, and improving patient safety.
How do I fill out the Texas Standard Prior Authorization Form?
+Filling out the Texas Standard Prior Authorization Form requires careful attention to detail. Follow the steps outlined in this article, including completing the patient information section, specifying the treatment or medication, providing medical justification, attaching supporting documentation, and signing and dating the form.