Prior authorization forms are a necessary part of the healthcare process, but they can often be a source of frustration for patients and healthcare providers alike. The Sunshine Prior Authorization Form is one such example, requiring detailed information and documentation before a patient can receive certain treatments or medications. However, with the right guidance and resources, navigating this form can be made much easier.
Understanding the Sunshine Prior Authorization Form

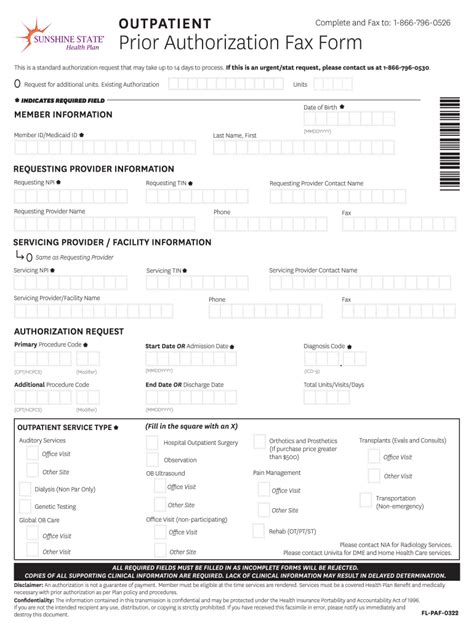
The Sunshine Prior Authorization Form is a standardized form used by healthcare providers and insurance companies to request prior authorization for certain medical treatments or medications. This form is typically required for patients who are seeking coverage for medications or treatments that are considered experimental, high-risk, or high-cost. The form requires detailed information about the patient's medical condition, treatment history, and other relevant factors.
Benefits of Using the Sunshine Prior Authorization Form
While the Sunshine Prior Authorization Form may seem like a hassle, it actually provides several benefits to patients and healthcare providers. For one, it helps ensure that patients receive the most effective and cost-efficient treatment for their condition. By requiring detailed information and documentation, the form helps healthcare providers and insurance companies make informed decisions about coverage. Additionally, the form helps to reduce the risk of adverse reactions or interactions with other medications.
How to Complete the Sunshine Prior Authorization Form

Completing the Sunshine Prior Authorization Form can seem daunting, but breaking it down into smaller sections can make it more manageable. Here are some steps to follow:
- Patient Information: Start by filling out the patient's demographic information, including name, date of birth, and contact information.
- Medical Condition: Provide a detailed description of the patient's medical condition, including diagnosis, symptoms, and treatment history.
- Treatment Request: Clearly state the treatment or medication being requested, including dosage and frequency.
- Clinical Rationale: Provide a clinical rationale for the requested treatment, including supporting documentation such as medical literature or clinical trials.
- Alternative Treatments: List any alternative treatments that have been tried or considered, including reasons for rejecting them.
- Supporting Documentation: Attach any supporting documentation, such as medical records, test results, or letters from other healthcare providers.
Tips for Healthcare Providers
Healthcare providers can make the prior authorization process easier by following these tips:
- Use clear and concise language: Avoid using medical jargon or complex terminology that may confuse the insurance company or patient.
- Provide detailed documentation: Include all relevant medical records, test results, and supporting documentation to help support the treatment request.
- Follow up: Follow up with the insurance company to ensure that the form has been received and is being processed.
Common Mistakes to Avoid

When completing the Sunshine Prior Authorization Form, there are several common mistakes to avoid. These include:
- Incomplete information: Failing to provide complete and accurate information can delay or even deny coverage.
- Lack of supporting documentation: Failing to provide supporting documentation can make it difficult to justify the treatment request.
- Inconsistent information: Providing inconsistent information can raise red flags and delay the approval process.
How to Expedite the Prior Authorization Process
While the prior authorization process can take time, there are steps that healthcare providers and patients can take to expedite it. These include:
- Submit complete and accurate information: Make sure to provide all required information and documentation upfront.
- Use electronic submission: Many insurance companies offer electronic submission options, which can speed up the process.
- Follow up: Follow up with the insurance company to ensure that the form has been received and is being processed.
Conclusion and Next Steps

In conclusion, the Sunshine Prior Authorization Form may seem daunting, but with the right guidance and resources, it can be made much easier. By understanding the benefits and requirements of the form, healthcare providers and patients can navigate the prior authorization process with ease. By following the tips and best practices outlined above, healthcare providers can help ensure that their patients receive the treatment they need in a timely and efficient manner.
We encourage you to share your experiences and tips for navigating the Sunshine Prior Authorization Form in the comments below. Additionally, if you have any questions or concerns about the form or the prior authorization process, please don't hesitate to reach out.
FAQ Section:
What is the Sunshine Prior Authorization Form?
+The Sunshine Prior Authorization Form is a standardized form used by healthcare providers and insurance companies to request prior authorization for certain medical treatments or medications.
What information is required on the Sunshine Prior Authorization Form?
+The form requires detailed information about the patient's medical condition, treatment history, and other relevant factors.
How long does the prior authorization process typically take?
+The prior authorization process can take anywhere from a few days to several weeks, depending on the complexity of the request and the efficiency of the insurance company.