Healthcare providers and patients often encounter the daunting task of navigating prior authorization forms, which can delay access to necessary medications and treatments. The Silverscript Prior Auth Form is no exception. However, understanding the process and having a clear guide can significantly reduce the administrative burden and expedite the approval process.
In this article, we will delve into the world of prior authorization, explore the specifics of the Silverscript Prior Auth Form, and provide a step-by-step guide to help you navigate the process with ease. Whether you are a healthcare provider, a patient, or a caregiver, this comprehensive guide aims to empower you with the knowledge you need to streamline the prior authorization process.
What is Prior Authorization?

Prior authorization is a process used by health insurance providers to determine whether a particular treatment, medication, or service is medically necessary and covered under the patient's insurance plan. This process is also known as pre-certification or pre-authorization. The goal of prior authorization is to ensure that patients receive necessary and effective treatments while minimizing unnecessary costs.
Why is Prior Authorization Necessary?
Prior authorization is essential for several reasons:
- Cost control: By reviewing treatment plans and medications before they are administered, insurance providers can prevent unnecessary costs and ensure that patients receive the most cost-effective treatments.
- Quality of care: Prior authorization ensures that patients receive evidence-based treatments that are medically necessary and effective.
- Patient safety: By reviewing treatment plans, insurance providers can identify potential risks and ensure that patients are not exposed to unnecessary harm.
Silverscript Prior Auth Form: Overview

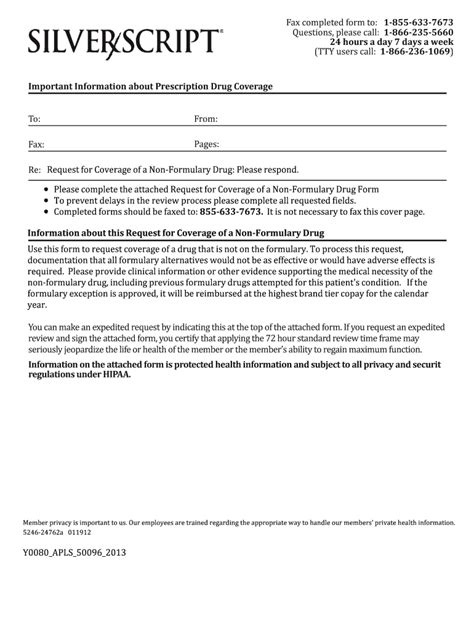
The Silverscript Prior Auth Form is a specific type of prior authorization form used by Silverscript, a prescription drug plan provider. This form is used to request prior authorization for medications, treatments, or services that require pre-approval before they can be covered under the patient's insurance plan.
What Information is Required on the Silverscript Prior Auth Form?
The Silverscript Prior Auth Form requires the following information:
- Patient demographics: Patient name, date of birth, and insurance ID number.
- Prescriber information: Prescriber name, contact information, and National Provider Identifier (NPI) number.
- Medication or treatment information: Medication name, dosage, frequency, and duration of treatment.
- Medical justification: A brief explanation of the medical necessity of the treatment or medication.
- Clinical documentation: Supporting clinical documentation, such as lab results, medical records, or test results.
Step-by-Step Guide to Completing the Silverscript Prior Auth Form

To complete the Silverscript Prior Auth Form, follow these steps:
- Gather required information: Collect all necessary information, including patient demographics, prescriber information, medication or treatment information, and clinical documentation.
- Complete the form: Fill out the form accurately and thoroughly, making sure to include all required information.
- Submit the form: Submit the completed form to Silverscript via fax, email, or online portal.
- Follow up: Follow up with Silverscript to ensure that the form has been received and is being processed.
Tips for Streamlining the Process
To streamline the prior authorization process, consider the following tips:
- Use electronic submissions: Submit the form electronically to reduce processing time and increase efficiency.
- Ensure accuracy: Double-check the form for accuracy and completeness to avoid delays.
- Provide supporting documentation: Include all necessary clinical documentation to support the request.
Common Challenges and Solutions

Despite the best efforts, prior authorization can be a challenging process. Here are some common challenges and solutions:
- Delays in processing: Solution: Follow up with Silverscript to ensure that the form has been received and is being processed.
- Incomplete or inaccurate forms: Solution: Double-check the form for accuracy and completeness before submission.
- Lack of clinical documentation: Solution: Include all necessary clinical documentation to support the request.
Conclusion: Taking Control of the Prior Authorization Process

By understanding the prior authorization process and using the Silverscript Prior Auth Form guide, you can take control of the process and reduce the administrative burden. Remember to stay organized, ensure accuracy, and provide supporting documentation to streamline the process. With practice and patience, you can master the prior authorization process and ensure that patients receive the necessary treatments and medications in a timely and efficient manner.
We hope this comprehensive guide has empowered you with the knowledge you need to navigate the Silverscript Prior Auth Form process with ease. Share your experiences, tips, and questions in the comments below!
What is the purpose of prior authorization?
+Prior authorization is used to determine whether a particular treatment, medication, or service is medically necessary and covered under the patient's insurance plan.
What information is required on the Silverscript Prior Auth Form?
+The Silverscript Prior Auth Form requires patient demographics, prescriber information, medication or treatment information, medical justification, and clinical documentation.
How can I streamline the prior authorization process?
+To streamline the process, use electronic submissions, ensure accuracy, and provide supporting documentation.