Streamlining prescription approvals is a crucial aspect of modern healthcare, as it enables patients to access necessary medications quickly and efficiently. One key component of this process is the prior authorization (prior auth) form. In this article, we will delve into the world of prior auth forms, exploring their importance, benefits, and steps to create an effective prior auth process.
Understanding Prior Authorization Forms

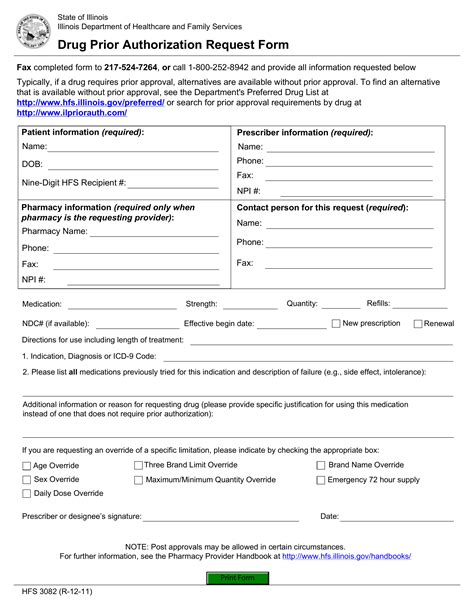
Prior authorization forms are documents used by healthcare providers to request approval from insurance companies or payers for specific treatments, medications, or medical services. These forms are designed to ensure that patients receive necessary care while also controlling healthcare costs. By reviewing prior auth requests, payers can verify the medical necessity of a treatment and ensure that it aligns with their coverage policies.
Why Prior Auth Forms Matter
Prior auth forms play a vital role in the healthcare system, as they help to:
- Ensure patient safety by verifying the appropriateness of a treatment
- Control healthcare costs by preventing unnecessary or duplicate treatments
- Improve communication between healthcare providers and payers
- Enhance the overall efficiency of the healthcare system
The Benefits of Streamlining Prior Auth Approvals

Streamlining prior auth approvals can have a significant impact on both healthcare providers and patients. Some of the key benefits include:
- Reduced administrative burden on healthcare providers
- Faster approval times, enabling patients to access necessary treatments more quickly
- Improved patient satisfaction and outcomes
- Enhanced collaboration between healthcare providers and payers
Steps to Create an Effective Prior Auth Process
To create an effective prior auth process, healthcare providers and payers should follow these steps:
- Clearly define prior auth requirements: Establish clear guidelines for prior auth requests, including the necessary documentation and information required.
- Implement an electronic prior auth system: Utilize electronic prior auth systems to streamline the submission and review process.
- Assign dedicated staff: Designate specific staff members to manage prior auth requests and ensure timely follow-up.
- Establish open communication channels: Foster open communication between healthcare providers and payers to resolve any issues or concerns.
- Monitor and evaluate the prior auth process: Regularly review the prior auth process to identify areas for improvement and optimize efficiency.
Best Practices for Prior Auth Forms

To create effective prior auth forms, healthcare providers and payers should follow these best practices:
- Use clear and concise language: Ensure that prior auth forms are easy to understand and complete.
- Include necessary documentation: Require all necessary documentation and information to support the prior auth request.
- Make forms easily accessible: Provide prior auth forms in multiple formats, including electronic and paper-based options.
- Regularly review and update forms: Periodically review and update prior auth forms to reflect changes in healthcare policies and regulations.
Common Challenges in Prior Auth Approvals
Despite the importance of prior auth forms, there are several common challenges that can hinder the approval process. These include:
- Inadequate documentation: Insufficient or incomplete documentation can lead to delayed or denied approvals.
- Lack of communication: Poor communication between healthcare providers and payers can result in misunderstandings and delays.
- Inefficient prior auth systems: Outdated or inefficient prior auth systems can slow down the approval process.
Overcoming Challenges in Prior Auth Approvals

To overcome common challenges in prior auth approvals, healthcare providers and payers can:
- Implement electronic prior auth systems: Utilize electronic prior auth systems to streamline the submission and review process.
- Establish clear communication channels: Foster open communication between healthcare providers and payers to resolve any issues or concerns.
- Provide thorough documentation: Ensure that all necessary documentation and information are included with the prior auth request.
The Future of Prior Auth Approvals
As the healthcare industry continues to evolve, prior auth approvals will play an increasingly important role in ensuring patient access to necessary treatments. To stay ahead of the curve, healthcare providers and payers should:
- Invest in digital technologies: Leverage digital technologies, such as artificial intelligence and machine learning, to optimize the prior auth process.
- Focus on patient-centered care: Prioritize patient-centered care by streamlining prior auth approvals and reducing administrative burdens.
- Collaborate and communicate: Foster collaboration and open communication between healthcare providers and payers to improve the prior auth process.
What is prior authorization?
+Prior authorization is a process used by healthcare providers to request approval from insurance companies or payers for specific treatments, medications, or medical services.
Why are prior auth forms important?
+Prior auth forms play a vital role in the healthcare system, as they help to ensure patient safety, control healthcare costs, and improve communication between healthcare providers and payers.
How can I streamline prior auth approvals?
+To streamline prior auth approvals, implement an electronic prior auth system, assign dedicated staff, and establish open communication channels between healthcare providers and payers.
By understanding the importance of prior auth forms and implementing effective prior auth processes, healthcare providers and payers can work together to streamline prescription approvals and improve patient outcomes. We invite you to share your thoughts and experiences with prior auth forms in the comments section below.