OptumRx, a leading pharmacy benefit management organization, requires prior authorization for certain medications, including Wegovy. Prior authorization is a process where your healthcare provider must obtain approval from OptumRx before prescribing a specific medication. In this article, we will guide you through the 5 easy steps to complete the OptumRx Wegovy prior authorization form.
Understanding the Importance of Prior Authorization

Prior authorization is a crucial step in ensuring that patients receive the most effective and cost-efficient treatment. It allows OptumRx to review the patient's medical history, current medications, and treatment plan to determine if the prescribed medication is medically necessary. By completing the prior authorization form, your healthcare provider can demonstrate that Wegovy is the best treatment option for you.
Step 1: Gather Required Information
Before starting the prior authorization process, your healthcare provider will need to gather some information. This includes:
- Your medical history, including any previous treatments or allergies
- Your current medications, including dosages and frequencies
- Your diagnosis and treatment plan
- Your demographic information, including name, date of birth, and contact information
Why is this information necessary?
OptumRx requires this information to assess the medical necessity of Wegovy and to ensure that it is the best treatment option for you. By providing accurate and complete information, your healthcare provider can help expedite the prior authorization process.
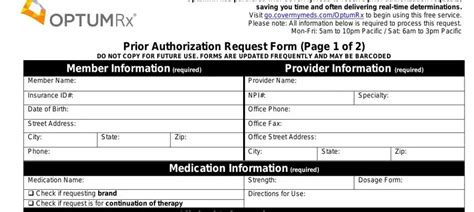
Step 2: Complete the Prior Authorization Form

The prior authorization form for Wegovy typically includes sections for:
- Patient demographics
- Medical history and diagnosis
- Current medications and treatment plan
- Prescription information, including dosage and frequency
- Healthcare provider information and signature
Your healthcare provider will need to complete the form accurately and thoroughly, providing all required information.
Tips for completing the form
- Make sure to fill out all required fields
- Provide accurate and complete information
- Attach any supporting documentation, such as medical records or test results
- Ensure that the form is signed and dated by your healthcare provider
Step 3: Submit the Prior Authorization Form
Once the prior authorization form is complete, your healthcare provider will need to submit it to OptumRx. This can typically be done via fax, mail, or online portal.
Submission methods
- Fax: [insert fax number]
- Mail: [insert mailing address]
- Online portal: [insert online portal link]
Make sure to follow the submission instructions carefully to ensure that the form is received and processed correctly.
Step 4: Wait for OptumRx Review

After submitting the prior authorization form, OptumRx will review the information to determine if Wegovy is medically necessary. This process typically takes a few days, but may take longer in some cases.
What happens during the review process?
- OptumRx will review the information provided on the prior authorization form
- They may request additional information or clarification
- They will assess the medical necessity of Wegovy based on your diagnosis and treatment plan
Step 5: Receive Approval or Denial
Once OptumRx has completed the review process, they will notify your healthcare provider of their decision. If approved, you will be able to receive Wegovy as prescribed. If denied, your healthcare provider may need to appeal the decision or explore alternative treatment options.
What to do if your request is denied
- Review the denial reason and explanation
- Discuss alternative treatment options with your healthcare provider
- Consider appealing the decision, if necessary
By following these 5 easy steps, you and your healthcare provider can complete the OptumRx Wegovy prior authorization form and ensure that you receive the treatment you need.
What is prior authorization?
+Prior authorization is a process where your healthcare provider must obtain approval from OptumRx before prescribing a specific medication.
Why is prior authorization required for Wegovy?
+Prior authorization is required to ensure that Wegovy is medically necessary and the best treatment option for you.
How long does the prior authorization process take?
+The prior authorization process typically takes a few days, but may take longer in some cases.