The Molina reconsideration form is a crucial document for individuals who have been denied coverage or reimbursement by Molina Healthcare, a leading health insurance provider. If you're one of the many people who have received a denial letter from Molina, you're likely feeling frustrated and unsure of what to do next. Fortunately, the Molina reconsideration form offers a way to appeal the decision and potentially overturn it. In this article, we'll provide a step-by-step guide on how to navigate the Molina reconsideration process, including what to expect, what information to include, and how to increase your chances of a successful appeal.
Understanding the Molina Reconsideration Process
Before we dive into the step-by-step guide, it's essential to understand the Molina reconsideration process. When you submit a claim to Molina, it's reviewed to determine whether the services or treatments are covered under your policy. If the claim is denied, you'll receive a denial letter explaining the reason for the decision. The Molina reconsideration form allows you to appeal this decision and provide additional information that may not have been considered during the initial review.

Step 1: Review the Denial Letter
The first step in the Molina reconsideration process is to carefully review the denial letter. This letter will outline the reason for the denial and provide information on how to appeal the decision. It's essential to understand the specific reason for the denial, as this will help you prepare your appeal.
Step 2: Gather Supporting Documentation
To increase your chances of a successful appeal, it's crucial to gather supporting documentation that addresses the reason for the denial. This may include:
- Medical records that demonstrate the necessity of the treatment or service
- Letters from your healthcare provider explaining the medical necessity of the treatment or service
- Test results or other medical evidence that supports your claim
- Receipts or invoices for the treatment or service
Make sure to organize your documentation in a clear and concise manner, as this will make it easier for the Molina review team to evaluate your appeal.
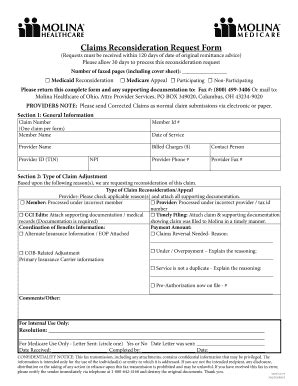
Step 3: Complete the Molina Reconsideration Form
Once you have gathered your supporting documentation, it's time to complete the Molina reconsideration form. This form will ask for information about your claim, including:
- Your name and policy number
- The date of the denial letter
- A description of the treatment or service that was denied
- The reason for the denial (as stated in the denial letter)
- A statement explaining why you disagree with the denial and why you believe the treatment or service should be covered
Make sure to complete the form accurately and thoroughly, as this will be the foundation of your appeal.
Step 4: Submit the Appeal
Once you have completed the Molina reconsideration form and gathered your supporting documentation, it's time to submit the appeal. You can submit the appeal via mail or fax, depending on your preference. Make sure to keep a copy of the appeal and supporting documentation for your records.

Step 5: Wait for a Decision
After submitting your appeal, it's time to wait for a decision from Molina. The review team will evaluate your appeal and make a decision based on the information provided. This process can take several weeks, so it's essential to be patient and allow the review team to complete their evaluation.
Tips for a Successful Appeal
While there are no guarantees of a successful appeal, there are several tips that can increase your chances of overturning the denial:
- Make sure to submit your appeal within the required timeframe (usually 60 days from the date of the denial letter)
- Provide clear and concise documentation that addresses the reason for the denial
- Ensure that your healthcare provider is involved in the appeal process and provides supporting documentation
- Follow up with Molina to ensure that your appeal has been received and is being processed
Common Mistakes to Avoid
When submitting a Molina reconsideration form, there are several common mistakes to avoid:
- Failing to submit the appeal within the required timeframe
- Not providing sufficient documentation to support your claim
- Not involving your healthcare provider in the appeal process
- Not following up with Molina to ensure that your appeal is being processed
By avoiding these common mistakes, you can increase your chances of a successful appeal and potentially overturn the denial.
Conclusion
The Molina reconsideration form is a crucial document for individuals who have been denied coverage or reimbursement by Molina Healthcare. By following the step-by-step guide outlined in this article, you can navigate the Molina reconsideration process and potentially overturn the denial. Remember to gather supporting documentation, complete the form accurately and thoroughly, and submit the appeal within the required timeframe. With persistence and the right information, you can increase your chances of a successful appeal.
What's Next?
If you're ready to submit a Molina reconsideration form, we encourage you to take the first step today. Gather your supporting documentation, complete the form, and submit your appeal. Don't let a denial letter stand in the way of receiving the coverage you need. Take control of your healthcare and appeal the decision.
What is the Molina reconsideration form?
+The Molina reconsideration form is a document that allows individuals to appeal a denial of coverage or reimbursement by Molina Healthcare.
How do I submit a Molina reconsideration form?
+You can submit the appeal via mail or fax, depending on your preference. Make sure to keep a copy of the appeal and supporting documentation for your records.
What information do I need to include in the Molina reconsideration form?
+You'll need to include information about your claim, including your name and policy number, the date of the denial letter, a description of the treatment or service that was denied, and a statement explaining why you disagree with the denial.