Molina Healthcare is a well-established health insurance company that provides coverage to millions of people across the United States. As part of its commitment to delivering high-quality care, Molina has implemented a prior authorization process to ensure that patients receive the most effective treatments while also controlling healthcare costs. The Molina prior auth form WA is a crucial document that healthcare providers must complete to request prior authorization for certain medical services or treatments.
However, filling out the Molina prior auth form WA can be a daunting task, especially for those who are new to the process. In this article, we will break down the process into 5 easy steps to help healthcare providers complete the form accurately and efficiently.
Step 1: Gather Required Information

Before starting to fill out the Molina prior auth form WA, it's essential to gather all the required information. This includes:
- Patient's demographic information, such as name, date of birth, and contact details
- Patient's insurance information, including policy number and group number
- Provider's information, including name, address, and contact details
- Details of the requested service or treatment, including CPT codes and diagnosis codes
- Supporting documentation, such as medical records and test results
Having all the necessary information readily available will make the process much smoother and reduce the likelihood of errors.
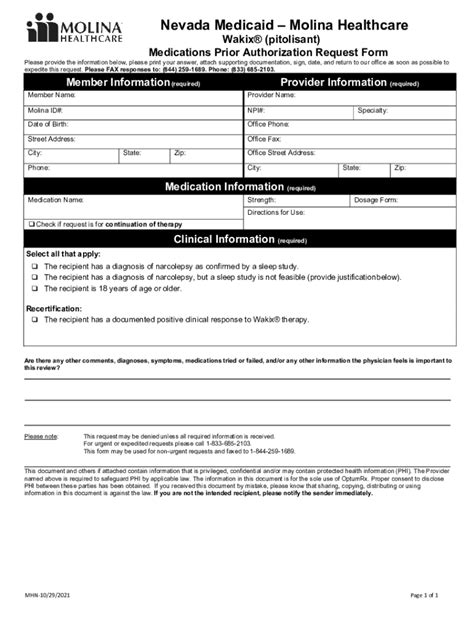
Step 2: Complete Section 1 - Patient Information
Section 1 - Patient Information
The first section of the Molina prior auth form WA requires patient demographic information. This includes:
- Patient's name
- Date of birth
- Contact details, including phone number and address
- Insurance information, including policy number and group number
Providers should ensure that all the information is accurate and up-to-date to avoid any delays or rejections.
Step 3: Complete Section 2 - Provider Information
Section 2 - Provider Information
The second section of the Molina prior auth form WA requires provider information. This includes:
- Provider's name
- Address
- Contact details, including phone number and fax number
- National Provider Identifier (NPI) number
Providers should ensure that all the information is accurate and up-to-date to avoid any delays or rejections.
Step 4: Complete Section 3 - Requested Service Information
Section 3 - Requested Service Information
The third section of the Molina prior auth form WA requires information about the requested service or treatment. This includes:
- CPT codes and diagnosis codes
- Description of the requested service or treatment
- Supporting documentation, such as medical records and test results
Providers should ensure that all the information is accurate and complete to avoid any delays or rejections.
Step 5: Review and Submit the Form

Once all the sections are complete, providers should review the form carefully to ensure that all the information is accurate and complete. The form should then be submitted to Molina via fax or online portal.
By following these 5 easy steps, healthcare providers can complete the Molina prior auth form WA accurately and efficiently. This will help to ensure that patients receive the necessary treatments and services while also controlling healthcare costs.
Best Practices for Completing the Molina Prior Auth Form WA
- Ensure that all the information is accurate and up-to-date
- Use the correct CPT codes and diagnosis codes
- Include supporting documentation, such as medical records and test results
- Review the form carefully before submitting it
- Submit the form via fax or online portal
By following these best practices, healthcare providers can avoid common mistakes and ensure that the prior authorization process runs smoothly.
Common Mistakes to Avoid
- Incomplete or inaccurate information
- Incorrect CPT codes and diagnosis codes
- Lack of supporting documentation
- Failure to review the form carefully before submitting it
- Submitting the form via the wrong channel
By avoiding these common mistakes, healthcare providers can ensure that the prior authorization process runs smoothly and efficiently.
Conclusion

Completing the Molina prior auth form WA is a crucial step in the prior authorization process. By following the 5 easy steps outlined in this article, healthcare providers can complete the form accurately and efficiently. Remember to gather all the required information, complete each section carefully, and review the form before submitting it. By following these best practices and avoiding common mistakes, healthcare providers can ensure that patients receive the necessary treatments and services while also controlling healthcare costs.
Share Your Thoughts
Have you ever completed the Molina prior auth form WA? What were your experiences? Share your thoughts and feedback in the comments section below.
FAQs
What is the Molina prior auth form WA?
+The Molina prior auth form WA is a document that healthcare providers must complete to request prior authorization for certain medical services or treatments.
How do I complete the Molina prior auth form WA?
+Follow the 5 easy steps outlined in this article to complete the form accurately and efficiently.
What are the common mistakes to avoid when completing the Molina prior auth form WA?
+Avoid common mistakes such as incomplete or inaccurate information, incorrect CPT codes and diagnosis codes, lack of supporting documentation, and failure to review the form carefully before submitting it.