Prior authorization is an essential step in the healthcare process, ensuring that patients receive the necessary treatments and medications while also controlling costs and promoting efficient use of resources. For healthcare providers and patients alike, navigating the prior authorization process can be complex and time-consuming. In this article, we will focus on Molina Complete Care prior authorization, providing a step-by-step guide to help streamline the process.
Molina Complete Care is a health plan that offers comprehensive coverage to its members, including prior authorization for certain treatments, medications, and services. Understanding the prior authorization process is crucial for healthcare providers and patients to ensure timely access to necessary care.
Understanding Prior Authorization

Prior authorization is a process where healthcare providers must obtain approval from the patient's health plan before providing certain treatments, medications, or services. This process helps ensure that patients receive necessary and cost-effective care while minimizing unnecessary procedures and medications.
Benefits of Prior Authorization
Prior authorization offers several benefits, including:
- Improved patient safety by reducing the risk of adverse reactions and unnecessary procedures
- Cost savings for patients and health plans by minimizing unnecessary treatments and medications
- Enhanced communication between healthcare providers and health plans, promoting more effective care coordination
Step 1: Verify Patient Eligibility

Before initiating the prior authorization process, healthcare providers must verify the patient's eligibility for Molina Complete Care. This involves checking the patient's membership status, coverage dates, and any applicable copays or deductibles.
To verify patient eligibility, healthcare providers can:
- Call Molina Complete Care's customer service department
- Check the patient's insurance card or membership documents
- Use Molina Complete Care's online portal or mobile app to verify eligibility
Required Information for Eligibility Verification
To verify patient eligibility, healthcare providers will need to provide the following information:
- Patient's name and date of birth
- Patient's Molina Complete Care membership ID
- Patient's coverage dates and applicable copays or deductibles
Step 2: Determine Prior Authorization Requirements

Once patient eligibility is verified, healthcare providers must determine if prior authorization is required for the proposed treatment, medication, or service. Molina Complete Care has specific prior authorization requirements for various treatments and medications.
To determine prior authorization requirements, healthcare providers can:
- Check Molina Complete Care's prior authorization list
- Use Molina Complete Care's online portal or mobile app to check prior authorization requirements
- Contact Molina Complete Care's customer service department for assistance
Prior Authorization Requirements for Common Treatments
Some common treatments and medications that may require prior authorization from Molina Complete Care include:
- Specialty medications
- Surgical procedures
- Hospital admissions
- Durable medical equipment
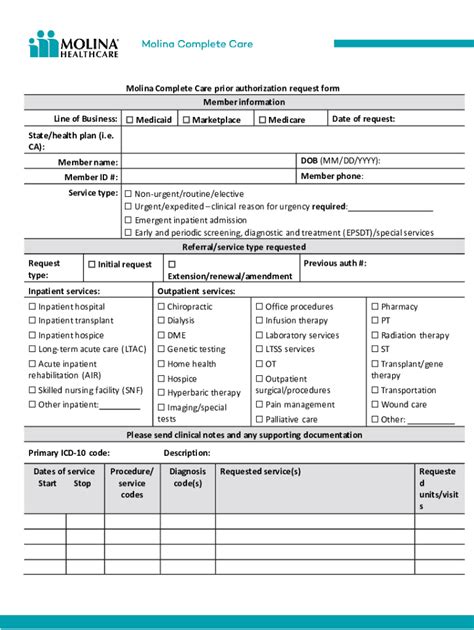
Step 3: Gather Required Documentation

If prior authorization is required, healthcare providers must gather the necessary documentation to support the request. This may include:
- Medical records and test results
- Treatment plans and medication lists
- Letters of medical necessity
- Supporting documentation from specialists or other healthcare providers
Required Documentation for Prior Authorization Requests
The required documentation for prior authorization requests may vary depending on the treatment or medication. However, common documentation includes:
- Patient's medical history and current condition
- Treatment plan and medication list
- Supporting documentation from specialists or other healthcare providers
Step 4: Submit Prior Authorization Request

Once the required documentation is gathered, healthcare providers can submit the prior authorization request to Molina Complete Care. This can be done:
- Online through Molina Complete Care's portal or mobile app
- By phone through Molina Complete Care's customer service department
- By fax or mail
Submitting Prior Authorization Requests Online
To submit prior authorization requests online, healthcare providers can:
- Log in to Molina Complete Care's portal or mobile app
- Select the patient's name and membership ID
- Choose the treatment or medication requiring prior authorization
- Upload the required documentation
Step 5: Receive Prior Authorization Decision

After submitting the prior authorization request, Molina Complete Care will review the request and make a determination. The decision will be communicated to the healthcare provider and patient.
Understanding Prior Authorization Decisions
Prior authorization decisions may be:
- Approved: The treatment or medication is approved, and the patient can proceed with the proposed care.
- Denied: The treatment or medication is denied, and the patient may need to explore alternative options.
- Pending: The request is pending, and additional information or documentation may be required.
In conclusion, navigating the prior authorization process for Molina Complete Care can be complex, but by following these 5 easy steps, healthcare providers can ensure timely access to necessary care for their patients. By understanding the prior authorization process and requirements, healthcare providers can improve patient outcomes and reduce costs.
We hope this article has provided valuable insights into the Molina Complete Care prior authorization process. If you have any questions or comments, please feel free to share them below.
What is prior authorization?
+Prior authorization is a process where healthcare providers must obtain approval from the patient's health plan before providing certain treatments, medications, or services.
Why is prior authorization required?
+Prior authorization is required to ensure that patients receive necessary and cost-effective care while minimizing unnecessary procedures and medications.
How do I submit a prior authorization request?
+Prior authorization requests can be submitted online through Molina Complete Care's portal or mobile app, by phone through Molina Complete Care's customer service department, or by fax or mail.