Missouri Medicaid prior authorization can be a daunting task for healthcare providers, requiring extensive documentation and tedious paperwork. However, by implementing a few strategies, you can simplify the process, reduce the administrative burden, and ensure timely access to necessary treatments for your patients.
Understanding the Importance of Prior Authorization

Prior authorization is a critical step in the healthcare process, ensuring that patients receive medically necessary treatments while controlling costs and preventing unnecessary procedures. In Missouri, Medicaid prior authorization is mandatory for certain services, including pharmaceuticals, medical equipment, and specialized treatments. By streamlining the prior authorization process, healthcare providers can improve patient outcomes, reduce administrative costs, and enhance overall care quality.
1. Implementing Electronic Prior Authorization

Electronic prior authorization (ePA) is a paperless, digital process that enables healthcare providers to submit prior authorization requests electronically. This approach eliminates the need for manual paperwork, reducing errors and increasing the speed of approval. Missouri Medicaid has implemented ePA through various platforms, such as the Medicaid Management Information System (MMIS) and the Health Information Exchange (HIE). By adopting ePA, healthcare providers can simplify the prior authorization process, reduce administrative burdens, and improve patient care.
Benefits of Electronic Prior Authorization
• Reduced paperwork and administrative tasks • Faster approval times and improved patient access to care • Enhanced accuracy and reduced errors • Improved communication between healthcare providers and Medicaid
2. Standardizing Prior Authorization Forms and Templates

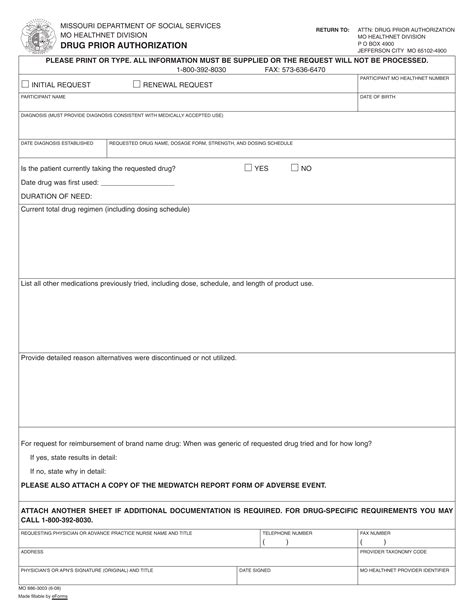
Standardizing prior authorization forms and templates can simplify the process, reduce errors, and improve the speed of approval. Missouri Medicaid provides standardized forms and templates for prior authorization requests, which can be accessed through the Medicaid website. Healthcare providers can also develop their own standardized forms and templates, ensuring consistency and accuracy in prior authorization submissions.
Benefits of Standardizing Prior Authorization Forms and Templates
• Improved accuracy and reduced errors • Enhanced consistency in prior authorization submissions • Reduced administrative burdens and improved efficiency • Improved patient care and outcomes
3. Leveraging Clinical Decision Support Tools

Clinical decision support (CDS) tools are designed to assist healthcare providers in making informed decisions about patient care. These tools can simplify the prior authorization process by providing real-time guidance on medical necessity, coverage, and prior authorization requirements. Missouri Medicaid has implemented CDS tools, such as the Medicaid CDS System, which provides healthcare providers with accurate and up-to-date information on prior authorization requirements.
Benefits of Leveraging Clinical Decision Support Tools
• Improved accuracy and reduced errors • Enhanced patient care and outcomes • Reduced administrative burdens and improved efficiency • Real-time guidance on prior authorization requirements
4. Streamlining Prior Authorization for High-Volume Services

High-volume services, such as pharmacy prior authorization, can be streamlined to simplify the process and reduce administrative burdens. Missouri Medicaid has implemented various initiatives to streamline high-volume services, including the use of automated prior authorization systems and centralized prior authorization processes.
Benefits of Streamlining High-Volume Services
• Reduced administrative burdens and improved efficiency • Improved patient care and outcomes • Enhanced accuracy and reduced errors • Faster approval times and improved patient access to care
5. Engaging in Ongoing Education and Training

Ongoing education and training are essential for healthcare providers to stay up-to-date on prior authorization requirements and processes. Missouri Medicaid offers various educational resources and training programs to assist healthcare providers in navigating the prior authorization process.
Benefits of Ongoing Education and Training
• Improved accuracy and reduced errors • Enhanced patient care and outcomes • Reduced administrative burdens and improved efficiency • Improved compliance with prior authorization requirements
By implementing these strategies, healthcare providers can simplify the Missouri Medicaid prior authorization process, reduce administrative burdens, and improve patient care. By leveraging electronic prior authorization, standardizing forms and templates, leveraging clinical decision support tools, streamlining high-volume services, and engaging in ongoing education and training, healthcare providers can ensure timely access to necessary treatments and improve patient outcomes.
What is prior authorization?
+Prior authorization is a process that requires healthcare providers to obtain approval from Medicaid before providing certain services or treatments.
What are the benefits of electronic prior authorization?
+Electronic prior authorization can reduce paperwork, improve accuracy, and enhance patient care.
How can I standardize prior authorization forms and templates?
+Healthcare providers can standardize prior authorization forms and templates by using Missouri Medicaid's standardized forms and templates or developing their own consistent forms and templates.