Receiving medical treatment can be a daunting experience, especially when it comes to navigating the complexities of insurance coverage. One crucial step in ensuring that your medical expenses are covered is completing the MHS prior authorization form. In this article, we will guide you through the 7 steps to complete the MHS prior authorization form, making the process as smooth as possible.
Medical billing and insurance claims can be overwhelming, but understanding the prior authorization process is essential for a hassle-free experience. Prior authorization is a process used by insurance companies to determine whether a particular treatment or medication is medically necessary and covered under your policy. In this article, we will delve into the world of MHS prior authorization, exploring its importance and providing a step-by-step guide on how to complete the form.

What is MHS Prior Authorization?
MHS prior authorization is a process used by Military Health System (MHS) to determine whether a particular treatment or medication is medically necessary and covered under your policy. The prior authorization process involves reviewing the patient's medical history, diagnosis, and treatment plan to ensure that the requested treatment is in line with the established medical guidelines.
Why is MHS Prior Authorization Important?
MHS prior authorization is crucial for several reasons:
- Ensures that patients receive medically necessary treatment
- Prevents unnecessary medical expenses
- Helps insurance companies manage healthcare costs
- Streamlines the medical billing and claims process
7 Steps to Complete MHS Prior Authorization Form
Now that we have understood the importance of MHS prior authorization, let's move on to the 7 steps to complete the form:

Step 1: Gather Required Documents
Before starting the prior authorization process, ensure that you have all the required documents, including:
- Patient's medical records
- Diagnosis and treatment plan
- Prescription or medication list
- Insurance policy documents
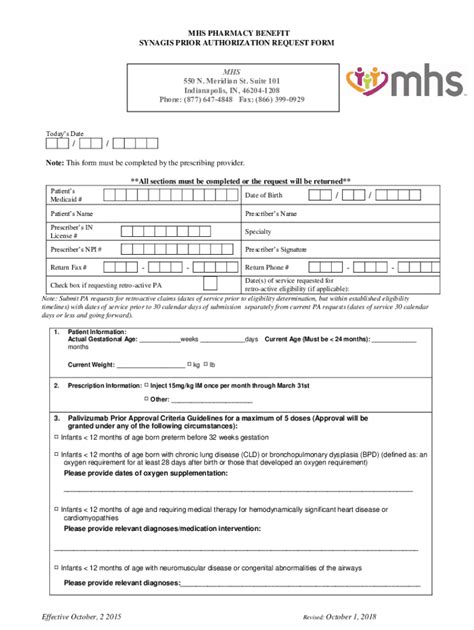
Step 2: Download and Review the MHS Prior Authorization Form
Download the MHS prior authorization form from the official website or obtain it from your healthcare provider. Review the form carefully, ensuring that you understand what information is required.

Step 3: Fill Out Patient Information
Fill out the patient's information section of the form, including:
- Name
- Date of birth
- Insurance policy number
- Contact information
Step 4: Provide Medical Information
Provide detailed medical information, including:
- Diagnosis
- Treatment plan
- Medication list
- Medical history
Step 5: Attach Supporting Documents
Attach all supporting documents, including:
- Medical records
- Prescription or medication list
- Insurance policy documents

Step 6: Review and Sign the Form
Review the form carefully, ensuring that all information is accurate and complete. Sign the form, acknowledging that the information provided is true and accurate.
Step 7: Submit the Form
Submit the completed form to the MHS prior authorization department, either by mail or online, depending on the preferred method of submission.
Tips for Completing the MHS Prior Authorization Form
To ensure a smooth prior authorization process, keep the following tips in mind:
- Ensure that all information is accurate and complete
- Attach all supporting documents
- Review the form carefully before submitting
- Submit the form well in advance of the treatment date
Conclusion
Completing the MHS prior authorization form is a crucial step in ensuring that your medical expenses are covered. By following the 7 steps outlined in this article, you can ensure a smooth prior authorization process. Remember to gather all required documents, fill out the form accurately, and attach all supporting documents. If you have any questions or concerns, don't hesitate to reach out to your healthcare provider or the MHS prior authorization department.
We hope this article has provided you with valuable insights into the MHS prior authorization process. If you have any questions or comments, please feel free to share them below.
What is MHS prior authorization?
+MHS prior authorization is a process used by Military Health System (MHS) to determine whether a particular treatment or medication is medically necessary and covered under your policy.
Why is MHS prior authorization important?
+MHS prior authorization is crucial for ensuring that patients receive medically necessary treatment, preventing unnecessary medical expenses, helping insurance companies manage healthcare costs, and streamlining the medical billing and claims process.
What documents are required for MHS prior authorization?
+The required documents for MHS prior authorization include patient's medical records, diagnosis and treatment plan, prescription or medication list, and insurance policy documents.