As the healthcare landscape continues to evolve, medical billing and insurance claims have become increasingly complex. One of the key components of this process is prior authorization, a critical step in ensuring that patients receive the necessary medical treatment while also controlling healthcare costs. For healthcare providers and medical billers in Illinois, navigating the Medicaid prior authorization process can be particularly challenging. In this article, we will break down the Illinois Medicaid prior authorization form process into five manageable steps.

Understanding the Importance of Prior Authorization
Prior authorization is a process that requires healthcare providers to obtain approval from the patient's insurance provider before administering certain medical treatments or prescribing specific medications. This step is crucial in ensuring that the treatment is medically necessary and that the patient is eligible for coverage. For Illinois Medicaid, prior authorization is an essential component of the claims process, and failure to comply can result in delayed or denied claims.
Step 1: Determine if Prior Authorization is Required
The first step in the Illinois Medicaid prior authorization process is to determine if prior authorization is required for the specific medical treatment or medication. Healthcare providers can check the Illinois Medicaid website or consult with the patient's insurance provider to determine if prior authorization is necessary. It's essential to note that prior authorization requirements can vary depending on the specific treatment or medication, as well as the patient's individual circumstances.
**Step 2: Gather Required Documentation**
Once it's determined that prior authorization is required, the next step is to gather the necessary documentation. This typically includes:
- Patient demographic information
- Medical history and treatment records
- Prescription or treatment plan
- Supporting documentation, such as lab results or medical imaging

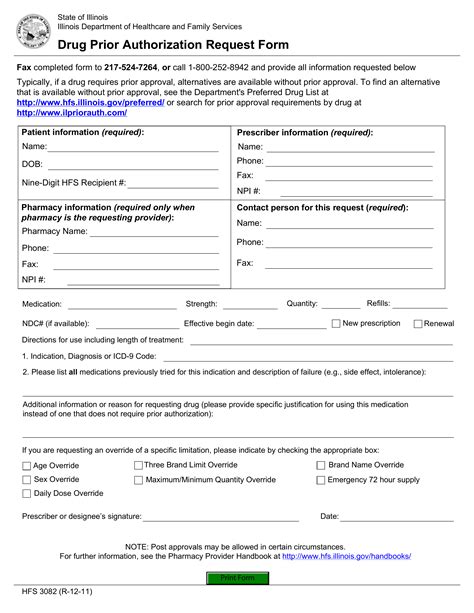
Step 3: Complete the Prior Authorization Form
The Illinois Medicaid prior authorization form can be downloaded from the Illinois Medicaid website or obtained through the patient's insurance provider. The form typically requires the following information:
- Patient demographic information
- Medical treatment or medication information
- Supporting documentation, such as medical records and lab results
- Healthcare provider information and signature
**Tips for Completing the Prior Authorization Form**
- Ensure all required fields are completed accurately and thoroughly
- Include all supporting documentation to avoid delays
- Sign and date the form to ensure authenticity
Step 4: Submit the Prior Authorization Form
Once the prior authorization form is complete, the next step is to submit it to the patient's insurance provider. This can typically be done via fax, email, or online portal. It's essential to follow the insurance provider's specific submission guidelines to avoid delays or rejection.

Step 5: Follow Up on Prior Authorization Status
After submitting the prior authorization form, it's crucial to follow up on the status of the request. This can be done by contacting the patient's insurance provider or checking the online portal. Healthcare providers should be prepared to provide additional information or supporting documentation if required.
**Conclusion: Streamlining the Prior Authorization Process**
The Illinois Medicaid prior authorization process can be complex and time-consuming, but by breaking it down into manageable steps, healthcare providers and medical billers can streamline the process and ensure timely approval. By understanding the importance of prior authorization, determining if prior authorization is required, gathering necessary documentation, completing the prior authorization form, submitting the form, and following up on the status, healthcare providers can ensure that patients receive the necessary medical treatment while also controlling healthcare costs.

We invite you to share your experiences and tips for navigating the Illinois Medicaid prior authorization process in the comments section below. If you have any questions or need further clarification on any of the steps, please don't hesitate to ask.
What is prior authorization, and why is it required?
+Prior authorization is a process that requires healthcare providers to obtain approval from the patient's insurance provider before administering certain medical treatments or prescribing specific medications. This step is crucial in ensuring that the treatment is medically necessary and that the patient is eligible for coverage.
How do I determine if prior authorization is required for a specific treatment or medication?
+Healthcare providers can check the Illinois Medicaid website or consult with the patient's insurance provider to determine if prior authorization is necessary.
What documentation is required for the prior authorization form?
+The prior authorization form typically requires patient demographic information, medical history and treatment records, prescription or treatment plan, and supporting documentation, such as lab results or medical imaging.