When dealing with medical billing and insurance claims, it's not uncommon to encounter errors or disagreements with insurance providers. For individuals covered under the Government Employees Health Association (GEHA) plan, understanding the appeals process is crucial in resolving such issues. Filing a GEHA provider appeal form can seem daunting, but breaking down the process into manageable steps can make it more approachable. Here's a comprehensive guide to help navigate the appeals process.
Understanding the Importance of Appeals
Appeals are an essential part of the healthcare billing process, allowing patients and providers to dispute denied claims or incorrect payments. In the context of GEHA, appeals can help resolve issues related to claim denials, underpayments, or disagreements with the insurance provider's decisions. By understanding the appeals process, individuals can ensure they receive the coverage they are entitled to.

Step 1: Review the Claim Decision
Before initiating the appeals process, it's essential to review the claim decision carefully. Ensure you understand the reasons for the denial or underpayment. Check for any errors in the claim submission, such as incorrect coding or missing information. Verify that the claim was submitted within the required timeframe. This review will help you identify the root cause of the issue and determine the best course of action.
Step 2: Gather Supporting Documentation
To build a strong appeal, it's crucial to gather supporting documentation. This may include:
- Medical records and test results
- Billing statements and invoices
- Claim forms and correspondence with GEHA
- Any additional documentation that supports your appeal
Organize the documents in a clear and concise manner, making it easy to reference specific information. Ensure that all documents are up-to-date and relevant to the appeal.

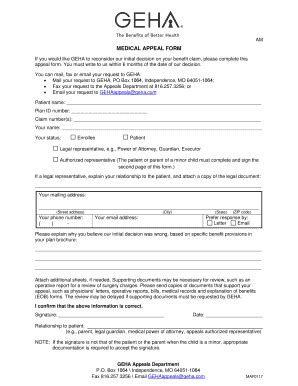
Step 3: Complete the GEHA Provider Appeal Form
The GEHA provider appeal form is a critical component of the appeals process. Ensure you complete the form accurately and thoroughly. Provide clear and concise explanations for the appeal, including:
- A detailed description of the issue
- The specific reason for the appeal
- Any relevant supporting documentation
Be sure to sign and date the form, as this will serve as a formal request for appeal.
Step 4: Submit the Appeal
Once the appeal form is complete, submit it to GEHA according to their guidelines. This may involve mailing or faxing the form, along with supporting documentation. Ensure you retain a copy of the appeal and supporting documents for your records.
Step 5: Follow Up and Escalate (If Necessary)
After submitting the appeal, follow up with GEHA to ensure it has been received and is being processed. If the appeal is denied or partially approved, you may need to escalate the issue to a higher level of review. This may involve submitting additional documentation or providing further clarification on the issue.

Best Practices for Filing a GEHA Provider Appeal Form
When filing a GEHA provider appeal form, keep the following best practices in mind:
- Ensure accuracy and completeness when completing the appeal form
- Provide clear and concise explanations for the appeal
- Include relevant supporting documentation
- Retain a copy of the appeal and supporting documents for your records
- Follow up with GEHA to ensure the appeal has been received and is being processed
By following these steps and best practices, individuals can effectively navigate the GEHA appeals process and resolve issues related to claim denials or underpayments.

Conclusion
Filing a GEHA provider appeal form can seem daunting, but by breaking down the process into manageable steps, individuals can effectively navigate the appeals process. Remember to review the claim decision carefully, gather supporting documentation, complete the appeal form accurately, submit the appeal, and follow up as necessary. By following these steps and best practices, individuals can ensure they receive the coverage they are entitled to.

We hope this article has provided valuable insights into the GEHA appeals process. If you have any questions or concerns, please don't hesitate to comment below. Share your experiences or tips for navigating the appeals process, and help others benefit from your knowledge.
What is the purpose of the GEHA provider appeal form?
+The GEHA provider appeal form is used to dispute denied claims or underpayments, allowing patients and providers to resolve issues related to claim denials or incorrect payments.
How long does the GEHA appeals process typically take?
+The length of time for the GEHA appeals process can vary depending on the complexity of the issue and the speed of response from GEHA. It's essential to follow up with GEHA to ensure the appeal is being processed in a timely manner.