In the healthcare industry, prior authorization (PA) is a crucial process that ensures patients receive necessary treatments while also controlling costs and promoting safe prescribing practices. Gainwell is a leading healthcare technology company that provides a range of solutions, including prior authorization tools, to streamline healthcare operations. In this article, we will delve into the world of Gainwell prior authorization forms, exploring the importance of PA, the benefits of using Gainwell's solutions, and providing a step-by-step guide on how to navigate the approval process.
Understanding Prior Authorization
Prior authorization is a process used by healthcare providers and payers to determine whether a specific treatment, medication, or service is medically necessary and covered under a patient's insurance plan. The PA process involves submitting a request to the payer, providing necessary documentation, and awaiting approval before proceeding with treatment. This process helps prevent unnecessary costs, reduces waste, and ensures that patients receive evidence-based care.
The Benefits of Gainwell Prior Authorization Solutions
Gainwell's prior authorization solutions are designed to simplify the PA process, reducing administrative burdens and improving patient outcomes. By leveraging Gainwell's technology, healthcare providers and payers can:
- Streamline the PA process, reducing approval times and improving patient access to care
- Automate documentation and data collection, minimizing errors and reducing administrative costs
- Enhance transparency and communication, ensuring that all stakeholders are informed and up-to-date on the status of PA requests
- Improve compliance with regulatory requirements and industry standards

Gainwell Prior Authorization Form: A Step-by-Step Guide
To navigate the Gainwell prior authorization form approval process, follow these steps:
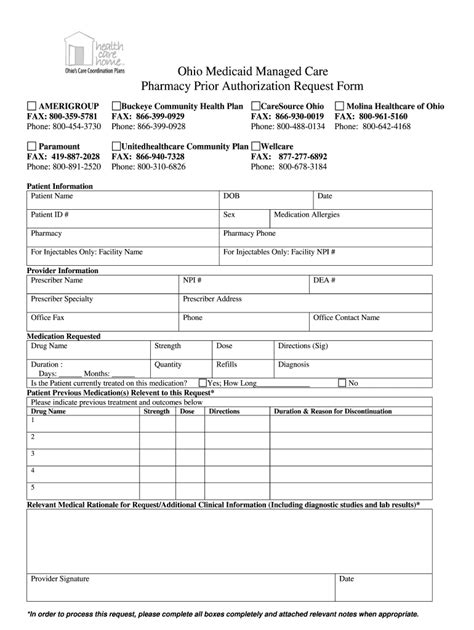
- Determine the type of prior authorization required: Identify the specific treatment, medication, or service that requires PA and determine the type of PA needed (e.g., medical, pharmacy, or behavioral health).
- Gather necessary documentation: Collect all relevant medical records, test results, and other supporting documentation required for the PA request.
- Complete the Gainwell prior authorization form: Fill out the Gainwell prior authorization form, ensuring that all required fields are completed accurately and thoroughly.
- Submit the PA request: Submit the completed form and supporting documentation to Gainwell's prior authorization platform or via fax/email.
- Track the status of the PA request: Monitor the status of the PA request through Gainwell's online portal or by contacting their customer support team.
Common Challenges and Solutions
While the Gainwell prior authorization form approval process is designed to be efficient and user-friendly, challenges can arise. Here are some common issues and solutions:
- Incomplete or inaccurate documentation: Ensure that all required documentation is complete and accurate to avoid delays or denials.
- Technical issues: Contact Gainwell's technical support team to resolve any technical issues or system errors.
- Delays in approval: Follow up with Gainwell's customer support team to inquire about the status of the PA request and ensure that all necessary documentation has been received.

Best Practices for Gainwell Prior Authorization Forms
To ensure a smooth and efficient PA process, follow these best practices:
- Use the most up-to-date Gainwell prior authorization form: Ensure that you are using the latest version of the form to avoid any errors or omissions.
- Complete all required fields: Ensure that all required fields are completed accurately and thoroughly to avoid delays or denials.
- Submit complete and accurate documentation: Ensure that all supporting documentation is complete, accurate, and relevant to the PA request.
Conclusion
Gainwell prior authorization forms are an essential tool for healthcare providers and payers, streamlining the PA process and improving patient outcomes. By following the step-by-step guide outlined in this article, healthcare professionals can navigate the approval process with ease, ensuring that patients receive necessary treatments in a timely and efficient manner. Remember to stay up-to-date with the latest Gainwell prior authorization form guidelines and best practices to ensure a smooth and efficient PA process.
What's Next?
We invite you to share your experiences and insights on using Gainwell prior authorization forms in the comments section below. Have you encountered any challenges or successes with the PA process? Share your stories and help us improve our content to better serve the healthcare community.
What is prior authorization, and why is it necessary?
+Prior authorization is a process used by healthcare providers and payers to determine whether a specific treatment, medication, or service is medically necessary and covered under a patient's insurance plan. It helps prevent unnecessary costs, reduces waste, and ensures that patients receive evidence-based care.
How long does the prior authorization process typically take?
+The prior authorization process can take anywhere from a few hours to several days or even weeks, depending on the complexity of the request and the speed of the healthcare provider and payer.
Can I appeal a denied prior authorization request?
+Yes, you can appeal a denied prior authorization request. Contact the payer's customer support team to inquire about the appeals process and submit additional documentation to support your appeal.