Ohio's healthcare system can be complex, especially when it comes to prior authorizations. If you're a healthcare provider or patient in Ohio, you may have encountered the Gainwell prior authorization form. In this article, we'll break down the process and provide a comprehensive guide to make it easier for you to navigate.
Prior authorizations are a crucial step in ensuring that patients receive the necessary treatment while also controlling healthcare costs. However, the process can be time-consuming and often leads to delays in care. The Gainwell prior authorization form is used by the Ohio Department of Medicaid to review and approve requests for certain medical services.

Understanding the Gainwell Prior Authorization Form
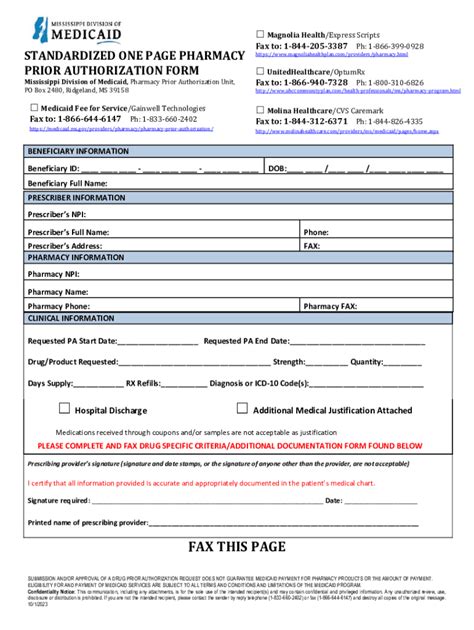
The Gainwell prior authorization form is used for a variety of medical services, including durable medical equipment, home health care, and prescription medications. The form requires healthcare providers to submit detailed information about the patient's condition, treatment plan, and medical history.
To streamline the process, it's essential to understand the different sections of the form and what information is required. The form typically includes:
- Patient demographics and contact information
- Healthcare provider information and credentials
- Description of the medical service or treatment being requested
- Supporting medical documentation, such as test results and medical records
- Estimated costs and duration of treatment
Benefits of Streamlining the Prior Authorization Process
Streamlining the prior authorization process can have numerous benefits for both healthcare providers and patients. Some of the advantages include:
- Reduced administrative burden on healthcare providers
- Faster approval times, resulting in quicker access to care for patients
- Improved communication between healthcare providers and payers
- Enhanced patient satisfaction and outcomes
- Reduced healthcare costs through more efficient use of resources

Steps to Complete the Gainwell Prior Authorization Form
Completing the Gainwell prior authorization form requires careful attention to detail and thorough documentation. Here are the steps to follow:
- Gather required information: Collect all necessary patient information, medical records, and supporting documentation.
- Choose the correct form: Ensure you're using the most up-to-date version of the Gainwell prior authorization form.
- Complete the form accurately: Fill out the form thoroughly and accurately, ensuring all required fields are completed.
- Attach supporting documentation: Include all relevant medical records, test results, and other supporting documentation.
- Submit the form: Submit the completed form to the Ohio Department of Medicaid or the designated payer.
Tips for Successful Prior Authorization
To increase the chances of successful prior authorization, consider the following tips:
- Submit complete and accurate information: Ensure all required fields are completed, and documentation is thorough.
- Use clear and concise language: Avoid using technical jargon or complex medical terminology.
- Include supporting documentation: Attach all relevant medical records and test results to support the request.
- Follow up: Verify receipt of the form and follow up on the status of the request.

Common Challenges and Solutions
Despite the importance of prior authorizations, the process can be plagued by challenges. Some common issues include:
- Delays in approval: Delays can result in delayed care and frustration for patients.
- Incomplete or inaccurate information: Incomplete or inaccurate information can lead to denials or delays.
- Lack of transparency: Lack of communication and transparency can lead to misunderstandings and frustration.
To overcome these challenges, consider the following solutions:
- Electronic submission: Submitting forms electronically can reduce delays and improve efficiency.
- Clear communication: Maintain open communication with patients, healthcare providers, and payers to ensure everyone is informed.
- Streamlined processes: Implement streamlined processes and workflows to reduce administrative burden.

Conclusion and Next Steps
The Gainwell prior authorization form can seem daunting, but by understanding the process and following the steps outlined in this article, you can make it easier to navigate. Remember to:
- Gather required information: Collect all necessary patient information and supporting documentation.
- Complete the form accurately: Fill out the form thoroughly and accurately, ensuring all required fields are completed.
- Submit the form: Submit the completed form to the Ohio Department of Medicaid or the designated payer.
By streamlining the prior authorization process, you can reduce administrative burden, improve patient satisfaction, and enhance healthcare outcomes.
We invite you to share your experiences and tips for navigating the Gainwell prior authorization form in the comments below.
What is the purpose of the Gainwell prior authorization form?
+The Gainwell prior authorization form is used by the Ohio Department of Medicaid to review and approve requests for certain medical services.
What information is required on the Gainwell prior authorization form?
+The form requires patient demographics, healthcare provider information, description of the medical service or treatment, supporting medical documentation, and estimated costs and duration of treatment.
How can I streamline the prior authorization process?
+Streamlining the prior authorization process can be achieved by submitting complete and accurate information, using clear and concise language, and including supporting documentation.