The Federal Employees Program (FEP) prior authorization form is a crucial document that healthcare providers must complete to ensure that their patients receive the necessary medical treatment. Completing this form can be a daunting task, especially for those who are new to the process. In this article, we will break down the FEP prior authorization form into five manageable steps, making it easier for healthcare providers to navigate the process.
What is the FEP Prior Authorization Form?
The FEP prior authorization form is a document that healthcare providers must complete to obtain approval from the patient's insurance provider before providing certain medical treatments or services. This form is used to ensure that the treatment or service is medically necessary and meets the insurance provider's coverage guidelines.
Step 1: Gather Required Information

The first step in completing the FEP prior authorization form is to gather all the required information. This includes:
- Patient's demographic information, such as name, date of birth, and insurance ID number
- Healthcare provider's information, including name, address, and National Provider Identifier (NPI) number
- Medical treatment or service being requested
- Medical records and test results that support the request
- Prescription medication list
Having all the necessary information readily available will make it easier to complete the form and reduce the likelihood of errors or delays.
Step 2: Determine the Type of Prior Authorization
Types of Prior Authorization
There are two types of prior authorization: medical and pharmacy. Medical prior authorization is required for medical treatments or services, such as surgeries or hospital stays. Pharmacy prior authorization is required for prescription medications.
- Medical prior authorization requires a healthcare provider to submit a request to the insurance provider before providing the medical treatment or service.
- Pharmacy prior authorization requires a healthcare provider to submit a request to the insurance provider before prescribing certain medications.
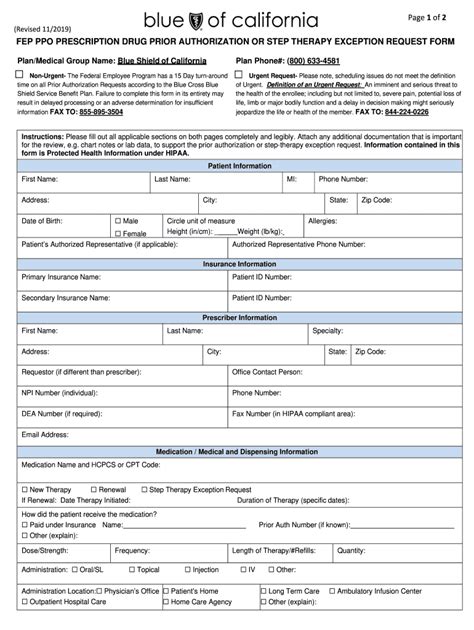
Step 3: Complete the Prior Authorization Form

Once you have determined the type of prior authorization required, the next step is to complete the FEP prior authorization form. The form will require you to provide detailed information about the patient, the medical treatment or service being requested, and the healthcare provider.
- Section 1: Patient Information
- Patient name and date of birth
- Insurance ID number and group number
- Contact information, including phone number and address
- Section 2: Healthcare Provider Information
- Healthcare provider name and NPI number
- Address and phone number
- Section 3: Medical Treatment or Service
- Description of the medical treatment or service being requested
- Diagnosis code and procedure code
- Start and end dates of treatment
- Section 4: Supporting Documentation
- Medical records and test results that support the request
- Prescription medication list
Step 4: Submit the Prior Authorization Form
Submission Options
There are several ways to submit the FEP prior authorization form, including:
- Fax: Fax the completed form to the insurance provider's fax number.
- Email: Email the completed form to the insurance provider's email address.
- Online Portal: Submit the completed form through the insurance provider's online portal.
- Mail: Mail the completed form to the insurance provider's address.
Step 5: Follow Up on the Prior Authorization Request

The final step is to follow up on the prior authorization request. This involves:
- Checking the status of the request online or by phone
- Responding to any additional information requests from the insurance provider
- Notifying the patient of the approval or denial of the request
By following these five steps, healthcare providers can ensure that they complete the FEP prior authorization form accurately and efficiently, reducing the risk of delays or denials.
Frequently Asked Questions
What is the FEP prior authorization form?
+The FEP prior authorization form is a document that healthcare providers must complete to obtain approval from the patient's insurance provider before providing certain medical treatments or services.
How long does it take to complete the FEP prior authorization form?
+The time it takes to complete the FEP prior authorization form varies depending on the complexity of the request and the availability of supporting documentation. On average, it can take 30 minutes to an hour to complete the form.
Can I submit the FEP prior authorization form electronically?
+Yes, many insurance providers offer online portals where healthcare providers can submit the FEP prior authorization form electronically.
We hope this article has provided valuable insights into the FEP prior authorization form and the steps required to complete it. If you have any further questions or concerns, please don't hesitate to reach out to us.