Tricare, the healthcare program for uniformed service members, retirees, and their families, relies on Express Scripts for pharmacy benefit management. One crucial step in accessing certain medications is obtaining prior authorization through the Express Scripts Tricare Prior Authorization Form. Understanding how to navigate this process can make a significant difference in accessing the care you need. In this article, we'll delve into the importance of prior authorization, the Express Scripts Tricare Prior Authorization Form, and provide 7 valuable tips for successfully completing and submitting the form.
Understanding Tricare and Prior Authorization

Tricare is designed to provide comprehensive healthcare coverage to its beneficiaries. However, to ensure that beneficiaries receive medically necessary care and to manage costs, certain treatments and medications may require prior authorization. This process involves getting approval from Express Scripts before receiving the medication. The Express Scripts Tricare Prior Authorization Form is a critical component of this process.
Why is Prior Authorization Important?
Prior authorization serves several purposes, including ensuring that medications are used appropriately and safely, controlling healthcare costs, and guaranteeing that beneficiaries receive the most effective treatment for their condition. It's a measure to balance access to necessary medications with the need to manage healthcare expenses.
Filling Out the Express Scripts Tricare Prior Authorization Form

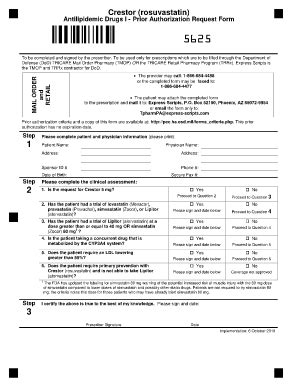
Successfully filling out the Express Scripts Tricare Prior Authorization Form requires careful attention to detail and a clear understanding of the process. Here are 7 tips to help you:
Tip 1: Gather All Necessary Information
Before starting the form, ensure you have all the required information at hand. This includes patient demographic information, medication details, diagnosis, and medical history. Having all the necessary documents and information ready will make the process smoother.
Tip 2: Choose the Right Form
Ensure you're using the correct version of the Express Scripts Tricare Prior Authorization Form. Forms are updated periodically, so using an outdated form can lead to delays or even rejection. Always check the Express Scripts website for the most current version.
Tip 3: Complete All Sections Carefully
Each section of the form is crucial, and incomplete sections can lead to delays. Pay special attention to sections requiring medical justification. This is where you explain why the medication is necessary for the patient's condition.
Tip 4: Provide Comprehensive Medical Justification
The medical justification section is key to a successful prior authorization. Clearly outline the medical necessity of the medication, including how it aligns with the patient's diagnosis and treatment plan. Use specific examples and reference clinical guidelines where possible.
Tip 5: Include Supporting Documentation
In addition to the form, submit any supporting documentation required. This can include patient records, test results, or letters from healthcare providers. Ensure these documents are legible and clearly labeled.
Tip 6: Submit the Form Correctly
Follow the submission instructions carefully. Forms can usually be submitted online, by fax, or by mail. Make sure to keep a copy of the form and any submitted documents for your records.
Tip 7: Follow Up on Your Request
After submitting the form, track its status. If you haven't received a decision within the expected timeframe (usually a few days to a couple of weeks), contact Express Scripts to inquire about the status of your request.
Conclusion
The Express Scripts Tricare Prior Authorization Form is a critical step in accessing necessary medications for Tricare beneficiaries. By understanding the importance of prior authorization and following these 7 tips, you can ensure a smoother process for yourself or your loved ones. Remember, prior authorization is a tool to ensure safe and effective treatment, and with the right approach, you can navigate this process with ease.
If you have any further questions or would like to share your experiences with the Express Scripts Tricare Prior Authorization Form, please don't hesitate to comment below.
What is the purpose of the Express Scripts Tricare Prior Authorization Form?
+The purpose of the Express Scripts Tricare Prior Authorization Form is to ensure that certain medications are used appropriately and safely by obtaining approval before they are dispensed.
How long does the prior authorization process typically take?
+The length of the prior authorization process can vary, but decisions are usually made within a few days to a couple of weeks after submitting the form and supporting documentation.
Can I appeal a prior authorization decision if it's denied?
+Yes, if a prior authorization request is denied, you can appeal the decision. The process for appealing will be outlined in the denial notification.