Excellus, a leading health insurance provider, requires prior authorization for certain medical treatments and medications to ensure that patients receive necessary care while managing costs. The Excellus prior authorization form is a crucial document that healthcare providers must complete to obtain approval for these services. In this article, we will discuss five ways to complete the Excellus prior authorization form efficiently and effectively.
Understanding the Excellus Prior Authorization Process

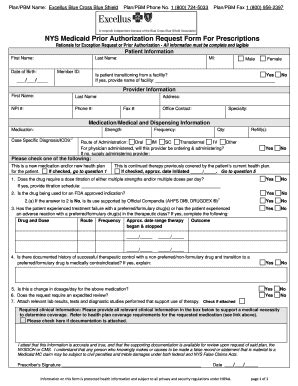
Prior authorization is a process used by health insurance companies to review medical treatment requests before approving or denying them. The goal is to ensure that patients receive necessary and cost-effective care. Excellus requires prior authorization for certain services, including medications, surgeries, and diagnostic tests. Healthcare providers must submit a prior authorization request form to Excellus for review and approval.
Why is Prior Authorization Important?
Prior authorization is essential for several reasons:
- It helps ensure that patients receive medically necessary treatment.
- It reduces unnecessary healthcare costs.
- It promotes communication between healthcare providers and insurance companies.
- It streamlines the claims process.
5 Ways to Complete the Excellus Prior Authorization Form

Completing the Excellus prior authorization form correctly is crucial to avoid delays or denials. Here are five ways to complete the form efficiently:
1. Gather Required Information
Before starting the prior authorization process, gather all necessary information, including:
- Patient demographics and insurance information
- Medical diagnosis and treatment history
- Prescription medication information
- Proposed treatment plan and supporting documentation
Tips for Gathering Information
- Use electronic health records (EHRs) to streamline data collection.
- Verify patient insurance information and benefits.
- Consult with colleagues or specialists to ensure accurate diagnosis and treatment plans.
2. Use the Correct Form and Submission Method
Excellus offers various prior authorization forms and submission methods, including online portals, fax, and mail. Choose the correct form and submission method to avoid delays.
Available Forms and Submission Methods
- Online portal: Excellus offers an online portal for submitting prior authorization requests.
- Fax: Fax the completed form to the designated number.
- Mail: Mail the completed form to the designated address.
3. Complete the Form Accurately and Thoroughly
Complete the prior authorization form accurately and thoroughly, including:
- Patient and provider information
- Medical diagnosis and treatment history
- Prescription medication information
- Proposed treatment plan and supporting documentation
Tips for Completing the Form
- Use clear and concise language.
- Provide supporting documentation, such as medical records and test results.
- Ensure all required fields are completed.
4. Submit the Form in a Timely Manner
Submit the prior authorization form in a timely manner to avoid delays or denials.
Submission Deadlines
- Excellus recommends submitting prior authorization requests at least 7-10 business days before the scheduled service date.
- Urgent requests can be submitted via fax or phone.
5. Follow Up on the Status
Follow up on the status of the prior authorization request to ensure timely approval or denial.
Tips for Following Up
- Check the online portal for status updates.
- Contact Excellus customer service for assistance.
- Be prepared to provide additional information or documentation.
Benefits of Efficient Prior Authorization

Efficient prior authorization offers several benefits, including:
- Reduced administrative burdens
- Improved patient satisfaction
- Enhanced care coordination
- Reduced costs
Streamlining the Prior Authorization Process
- Implement electronic prior authorization systems.
- Designate a prior authorization coordinator.
- Develop a prior authorization workflow.
Conclusion: Streamlining the Excellus Prior Authorization Process

Completing the Excellus prior authorization form efficiently and effectively is crucial to ensure timely approval or denial. By following the five ways outlined in this article, healthcare providers can streamline the prior authorization process, reduce administrative burdens, and improve patient satisfaction.
We invite you to share your experiences and tips for completing the Excellus prior authorization form in the comments section below. Your feedback will help others navigate this complex process.
What is the purpose of prior authorization?
+Prior authorization is a process used by health insurance companies to review medical treatment requests before approving or denying them. The goal is to ensure that patients receive necessary and cost-effective care.
What information is required for prior authorization?
+Required information includes patient demographics and insurance information, medical diagnosis and treatment history, prescription medication information, and proposed treatment plan and supporting documentation.
How can I submit a prior authorization request to Excellus?
+Excellus offers various prior authorization forms and submission methods, including online portals, fax, and mail. Choose the correct form and submission method to avoid delays.