The world of healthcare and insurance can be overwhelming, especially when it comes to navigating complex administrative tasks. One such task is enrolling in the CMS Edi (Electronic Data Interchange) program, which allows healthcare providers to electronically submit claims and receive payments from Medicare. In this article, we will break down the CMS Edi enrollment form and provide a simplified guide to help you navigate the sign-up process.
The importance of Edi in healthcare cannot be overstated. By adopting electronic data interchange, healthcare providers can streamline their claims submission process, reduce errors, and increase efficiency. Moreover, Edi helps to reduce administrative costs and improves the overall quality of care. However, the enrollment process can be daunting, especially for small healthcare providers or those who are new to Edi.

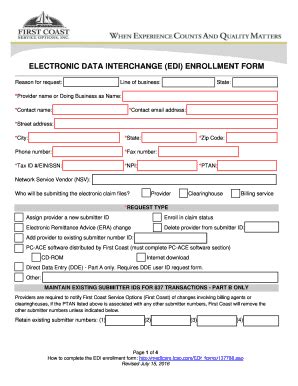
Understanding the CMS Edi Enrollment Form
The CMS Edi enrollment form is a critical step in the process of enrolling in the Edi program. The form requires healthcare providers to submit their demographic and administrative information, which is used to verify their identity and eligibility for Edi. The form typically includes sections for:
- Provider information, including name, address, and National Provider Identifier (NPI)
- Contact information, including phone number and email address
- Administrative information, including taxpayer identification number (TIN) and employer identification number (EIN)
- Edi setup information, including trading partner identification and interchange control number

Benefits of Edi Enrollment
Enrolling in the CMS Edi program offers numerous benefits to healthcare providers, including:
- Reduced administrative costs: Edi eliminates the need for manual claims submission and processing, reducing administrative costs and increasing efficiency.
- Faster payment: Edi enables healthcare providers to receive payments faster, as claims are processed electronically and payments are made directly to the provider's bank account.
- Improved accuracy: Edi reduces errors associated with manual claims submission, ensuring that claims are processed accurately and efficiently.
- Enhanced security: Edi ensures that sensitive patient information is protected and secure, reducing the risk of data breaches and cyber attacks.

A Step-by-Step Guide to CMS Edi Enrollment
To simplify the CMS Edi enrollment process, we have broken down the steps into a easy-to-follow guide:
- Determine eligibility: Verify that your healthcare organization is eligible for Edi enrollment. This includes checking that your organization has a valid NPI and TIN.
- Gather required documents: Collect all required documents, including provider information, contact information, and administrative information.
- Complete the enrollment form: Fill out the CMS Edi enrollment form accurately and completely, ensuring that all required information is included.
- Submit the enrollment form: Submit the completed enrollment form to the designated CMS Edi enrollment processing center.
- Verify enrollment: Verify that your enrollment has been successfully processed and that you have been assigned a trading partner identification.

Common Challenges and Solutions
Despite the benefits of Edi, many healthcare providers face challenges during the enrollment process. Some common challenges and solutions include:
- Incomplete or inaccurate information: Ensure that all required information is accurate and complete to avoid delays in the enrollment process.
- Technical difficulties: Contact the CMS Edi enrollment processing center for technical support and assistance with troubleshooting.
- Eligibility issues: Verify eligibility before starting the enrollment process to avoid delays or rejection.

Best Practices for Edi Enrollment
To ensure a smooth and efficient Edi enrollment process, follow these best practices:
- Plan ahead: Allow sufficient time for the enrollment process to avoid delays or last-minute complications.
- Seek support: Contact the CMS Edi enrollment processing center for technical support and assistance with troubleshooting.
- Verify information: Ensure that all required information is accurate and complete to avoid delays in the enrollment process.

By following these best practices and understanding the CMS Edi enrollment form, healthcare providers can navigate the sign-up process with ease and confidence. Don't hesitate to reach out for support and assistance – enroll in the CMS Edi program today and start streamlining your claims submission process!
We encourage you to share your experiences and tips for navigating the CMS Edi enrollment process in the comments below. Additionally, if you have any questions or concerns, please don't hesitate to ask. We're here to help!
What is the CMS Edi program?
+The CMS Edi program allows healthcare providers to electronically submit claims and receive payments from Medicare.
What are the benefits of Edi enrollment?
+Edi enrollment offers numerous benefits, including reduced administrative costs, faster payment, improved accuracy, and enhanced security.
How do I enroll in the CMS Edi program?
+To enroll in the CMS Edi program, follow the step-by-step guide outlined in this article, including determining eligibility, gathering required documents, completing the enrollment form, submitting the enrollment form, and verifying enrollment.