Understanding the CMS 1490s Claim Form: Importance and Benefits

The CMS 1490s claim form is a crucial document for healthcare providers to submit claims for reimbursement from the Centers for Medicare and Medicaid Services (CMS). It is essential for providers to understand the importance of this form and its benefits. In this article, we will provide a step-by-step guide on how to complete the CMS 1490s claim form, highlighting its significance, and explaining the working mechanisms.
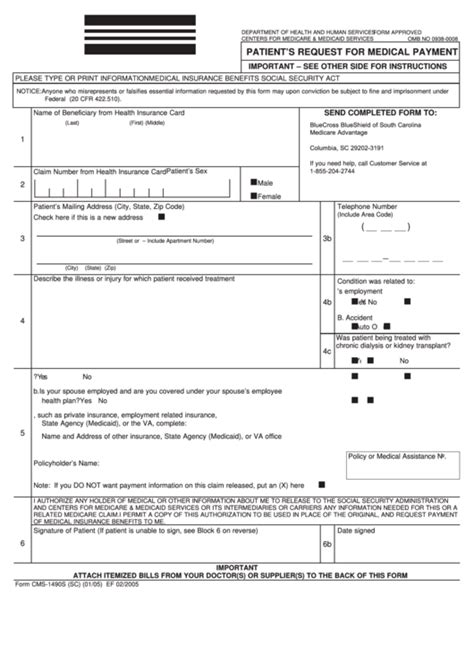
The CMS 1490s claim form is a standardized document used by healthcare providers to submit claims for reimbursement from CMS. The form requires providers to provide detailed information about the patient, the services rendered, and the charges for those services. The information provided on the form helps CMS to determine the eligibility of the claim and the amount of reimbursement due to the provider.
Why is the CMS 1490s Claim Form Important?
The CMS 1490s claim form is essential for healthcare providers to receive reimbursement for their services. Without a properly completed claim form, providers may experience delays or denials of payment, which can negatively impact their cash flow and financial stability. Moreover, the claim form provides valuable data for CMS to analyze and improve the Medicare and Medicaid programs.
Step-by-Step Guide to Completing the CMS 1490s Claim Form

To complete the CMS 1490s claim form, follow these steps:
Step 1: Gather Required Information
Before starting to complete the claim form, gather all the necessary information, including:
- Patient demographics and insurance information
- Dates of service and charges for each service rendered
- Procedure codes and diagnoses
- Supporting documentation, such as medical records and test results
Step 2: Fill Out the Patient Information Section
Complete the patient information section, including the patient's name, date of birth, and insurance information.
Step 3: Fill Out the Service Information Section
Complete the service information section, including the dates of service, procedure codes, and charges for each service rendered.
Step 4: Fill Out the Diagnoses Section
Complete the diagnoses section, including the patient's primary and secondary diagnoses.
Step 5: Fill Out the Supporting Documentation Section
Attach supporting documentation, such as medical records and test results, to the claim form.
Step 6: Review and Submit the Claim Form
Review the claim form for accuracy and completeness, and submit it to CMS for processing.
Tips for Accurate and Efficient Claim Form Completion
To ensure accurate and efficient claim form completion, follow these tips:
- Use a standardized template to complete the claim form
- Double-check the patient's insurance information and demographics
- Use correct procedure codes and diagnoses
- Attach supporting documentation, such as medical records and test results
- Review the claim form for accuracy and completeness before submitting it to CMS
CMS 1490s Claim Form: Common Errors and Solutions

Common errors on the CMS 1490s claim form can lead to delays or denials of payment. To avoid these errors, follow these solutions:
- Error: Incorrect patient information
- Solution: Double-check the patient's demographics and insurance information before completing the claim form.
- Error: Incorrect procedure codes or diagnoses
- Solution: Use a standardized template to complete the claim form, and double-check the procedure codes and diagnoses.
- Error: Missing supporting documentation
- Solution: Attach supporting documentation, such as medical records and test results, to the claim form.
Conclusion and Next Steps
In conclusion, the CMS 1490s claim form is a critical document for healthcare providers to submit claims for reimbursement from CMS. By following the step-by-step guide and tips provided in this article, providers can ensure accurate and efficient claim form completion. To stay up-to-date on the latest changes and updates to the CMS 1490s claim form, visit the CMS website or consult with a medical billing expert.
We invite you to share your experiences and tips on completing the CMS 1490s claim form in the comments section below. Your feedback will help us improve our content and provide more valuable information to our readers.
What is the CMS 1490s claim form?
+The CMS 1490s claim form is a standardized document used by healthcare providers to submit claims for reimbursement from the Centers for Medicare and Medicaid Services (CMS).
Why is the CMS 1490s claim form important?
+The CMS 1490s claim form is essential for healthcare providers to receive reimbursement for their services. Without a properly completed claim form, providers may experience delays or denials of payment.
How do I complete the CMS 1490s claim form?
+To complete the CMS 1490s claim form, follow the step-by-step guide provided in this article, and gather all the necessary information, including patient demographics and insurance information, dates of service and charges for each service rendered, procedure codes and diagnoses, and supporting documentation.