Understanding the Importance of Prior Authorization Forms

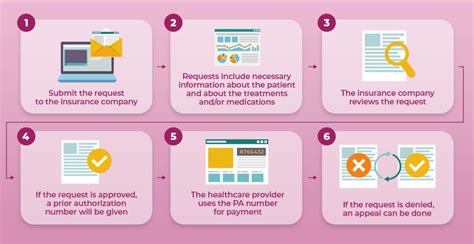
Prior authorization forms are a crucial part of the healthcare system, allowing healthcare providers to obtain approval from insurance companies before administering specific treatments or medications. The CCByqh Prior Authorization Form is one such document that requires careful completion to ensure that patients receive the necessary care. In this article, we will guide you through the process of completing the CCByqh Prior Authorization Form in 5 easy steps.
The CCByqh Prior Authorization Form is designed to streamline the prior authorization process, making it easier for healthcare providers to obtain approval for treatments and medications. However, completing the form correctly is essential to avoid delays or denials. By following the steps outlined in this article, you can ensure that the form is completed accurately and efficiently.
Why is Prior Authorization Important?
Prior authorization is essential in the healthcare system because it helps ensure that patients receive the most effective and cost-efficient treatment options. By requiring healthcare providers to obtain approval before administering certain treatments or medications, insurance companies can:
- Ensure that patients receive evidence-based treatments
- Reduce healthcare costs by avoiding unnecessary treatments
- Improve patient outcomes by ensuring that treatments are tailored to individual needs
Step 1: Gather Required Information

Before starting the CCByqh Prior Authorization Form, it is essential to gather all required information. This includes:
- Patient demographics, including name, date of birth, and insurance information
- Treatment or medication information, including dosage and frequency
- Diagnosis and medical history
- Healthcare provider information, including name and contact details
Having all the necessary information readily available will help you complete the form quickly and accurately.
What Information is Required for the CCByqh Prior Authorization Form?
The CCByqh Prior Authorization Form requires the following information:
- Patient name and date of birth
- Insurance information, including policy number and group number
- Treatment or medication information, including dosage and frequency
- Diagnosis and medical history
- Healthcare provider information, including name and contact details
Step 2: Complete Patient and Insurance Information

The first section of the CCByqh Prior Authorization Form requires patient and insurance information. This includes:
- Patient name and date of birth
- Insurance information, including policy number and group number
Ensure that this information is accurate and up-to-date, as any errors may delay or deny approval.
How to Complete the Patient and Insurance Information Section
To complete this section, follow these steps:
- Enter the patient's name and date of birth
- Enter the insurance policy number and group number
- Ensure that the information is accurate and up-to-date
Step 3: Complete Treatment or Medication Information

The next section of the CCByqh Prior Authorization Form requires treatment or medication information. This includes:
- Treatment or medication name
- Dosage and frequency
- Duration of treatment
Ensure that this information is accurate and up-to-date, as any errors may delay or deny approval.
How to Complete the Treatment or Medication Information Section
To complete this section, follow these steps:
- Enter the treatment or medication name
- Enter the dosage and frequency
- Enter the duration of treatment
- Ensure that the information is accurate and up-to-date
Step 4: Complete Diagnosis and Medical History

The next section of the CCByqh Prior Authorization Form requires diagnosis and medical history. This includes:
- Diagnosis code
- Medical history, including relevant illnesses or conditions
Ensure that this information is accurate and up-to-date, as any errors may delay or deny approval.
How to Complete the Diagnosis and Medical History Section
To complete this section, follow these steps:
- Enter the diagnosis code
- Enter the medical history, including relevant illnesses or conditions
- Ensure that the information is accurate and up-to-date
Step 5: Complete Healthcare Provider Information

The final section of the CCByqh Prior Authorization Form requires healthcare provider information. This includes:
- Healthcare provider name
- Contact details, including phone number and fax number
Ensure that this information is accurate and up-to-date, as any errors may delay or deny approval.
How to Complete the Healthcare Provider Information Section
To complete this section, follow these steps:
- Enter the healthcare provider name
- Enter the contact details, including phone number and fax number
- Ensure that the information is accurate and up-to-date
By following these 5 easy steps, you can complete the CCByqh Prior Authorization Form accurately and efficiently. Remember to gather all required information before starting the form, and ensure that all sections are completed correctly.
Conclusion: Completing the CCByqh Prior Authorization Form with Ease

Completing the CCByqh Prior Authorization Form can seem daunting, but by breaking it down into 5 easy steps, you can ensure that the form is completed accurately and efficiently. Remember to gather all required information, complete each section correctly, and review the form carefully before submitting it.
By following these steps, you can ensure that patients receive the necessary care and treatment, while also streamlining the prior authorization process.
What is the purpose of the CCByqh Prior Authorization Form?
+The CCByqh Prior Authorization Form is designed to streamline the prior authorization process, allowing healthcare providers to obtain approval from insurance companies before administering specific treatments or medications.
What information is required to complete the CCByqh Prior Authorization Form?
+The CCByqh Prior Authorization Form requires patient demographics, treatment or medication information, diagnosis and medical history, and healthcare provider information.
How long does it take to complete the CCByqh Prior Authorization Form?
+The time it takes to complete the CCByqh Prior Authorization Form will vary depending on the complexity of the treatment or medication and the availability of required information. However, by following the 5 easy steps outlined in this article, you can complete the form efficiently.