As a healthcare provider, navigating the complexities of Medicare Advantage plans can be a daunting task. One crucial aspect of these plans is prior authorization, which requires healthcare providers to obtain approval from the insurance company before providing certain treatments or services. CareFirst, a prominent health insurance provider, offers Medicare Advantage plans that require prior authorization for specific procedures. In this article, we will delve into the world of CareFirst Medicare Advantage prior authorization forms, exploring the process, benefits, and steps to ensure a smooth experience for both healthcare providers and patients.
Understanding Prior Authorization and Its Importance

Prior authorization is a critical process in healthcare that ensures patients receive necessary and cost-effective treatments. By requiring healthcare providers to obtain approval before administering certain procedures, insurance companies can:
- Control costs by avoiding unnecessary treatments
- Ensure patients receive evidence-based care
- Streamline the healthcare process by reducing administrative burdens
For healthcare providers, understanding the prior authorization process is vital to delivering quality care while minimizing delays and denials.
What is CareFirst Medicare Advantage Prior Authorization Form?

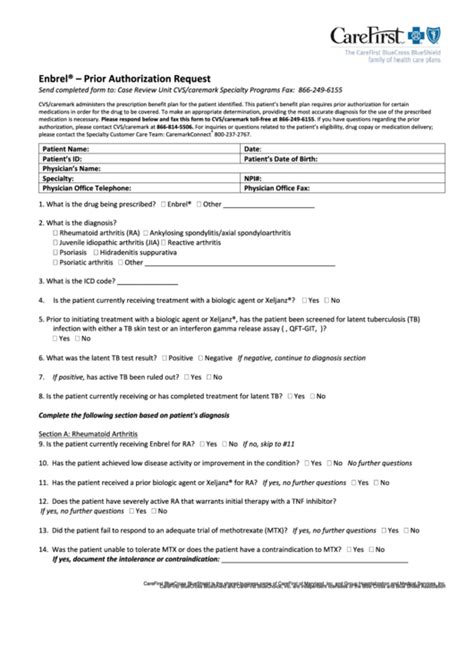
The CareFirst Medicare Advantage prior authorization form is a document that healthcare providers must submit to CareFirst to request approval for specific treatments or services. This form requires detailed information about the patient's condition, treatment plan, and medical history.
CareFirst Medicare Advantage prior authorization forms typically include:
- Patient demographics and insurance information
- Treatment details, including procedure codes and diagnoses
- Supporting medical documentation, such as test results and medical records
- Prescriber and provider information
By completing and submitting this form, healthcare providers can request prior authorization for various services, including:
- Medications
- Surgical procedures
- Diagnostic tests
- Durable medical equipment
Benefits of CareFirst Medicare Advantage Prior Authorization Form

The CareFirst Medicare Advantage prior authorization form offers several benefits for healthcare providers and patients:
- Streamlined process: The form provides a clear and structured way to request prior authorization, reducing administrative burdens and minimizing delays.
- Improved patient outcomes: By ensuring patients receive evidence-based care, prior authorization can lead to better health outcomes and reduced complications.
- Reduced costs: Prior authorization helps control costs by avoiding unnecessary treatments and tests.
- Enhanced patient safety: The form allows CareFirst to review and approve treatments, reducing the risk of adverse events and medication errors.
Steps to Complete CareFirst Medicare Advantage Prior Authorization Form

To complete the CareFirst Medicare Advantage prior authorization form, follow these steps:
- Gather required information: Collect patient demographics, insurance information, treatment details, and supporting medical documentation.
- Choose the correct form: Select the relevant prior authorization form for the specific treatment or service.
- Complete the form accurately: Fill out the form with precise and up-to-date information, ensuring all required fields are completed.
- Attach supporting documentation: Include relevant medical records, test results, and other supporting documentation to facilitate the review process.
- Submit the form: Send the completed form to CareFirst via fax, email, or online portal.
Common Mistakes to Avoid When Completing CareFirst Medicare Advantage Prior Authorization Form

To ensure a smooth prior authorization process, avoid the following common mistakes:
- Inaccurate or incomplete information: Double-check all fields for accuracy and completeness.
- Insufficient supporting documentation: Include all relevant medical records and test results to support the treatment request.
- Late submissions: Submit the form in a timely manner to avoid delays in treatment.
Conclusion
CareFirst Medicare Advantage prior authorization forms play a vital role in ensuring patients receive necessary and cost-effective treatments. By understanding the process, benefits, and steps to complete the form, healthcare providers can navigate the prior authorization process with ease. Remember to avoid common mistakes and submit the form accurately and on time to minimize delays and denials.
We invite you to share your experiences with CareFirst Medicare Advantage prior authorization forms in the comments below. Have you encountered any challenges or successes with the prior authorization process? Your insights will help us improve our content and provide valuable information to our readers.
What is prior authorization, and why is it required?
+Prior authorization is a process that requires healthcare providers to obtain approval from the insurance company before providing certain treatments or services. It is required to ensure patients receive necessary and cost-effective treatments, control costs, and streamline the healthcare process.
What information is required on the CareFirst Medicare Advantage prior authorization form?
+The form requires patient demographics, insurance information, treatment details, and supporting medical documentation, including test results and medical records.
How do I submit the CareFirst Medicare Advantage prior authorization form?
+The form can be submitted via fax, email, or online portal. Ensure you follow the correct submission process to avoid delays.