The healthcare industry is a complex and ever-evolving field, with numerous stakeholders working together to provide quality patient care. One crucial aspect of this process is prior authorization, a critical step in ensuring that patients receive the necessary treatment while also managing healthcare costs. In this article, we will delve into the specifics of the Blue Cross Blue Shield of Arizona prior auth form, its importance, and the steps involved in the process.
The Importance of Prior Authorization
Prior authorization is a process used by health insurance companies to determine whether a specific treatment, medication, or service is medically necessary and covered under a patient's insurance plan. This step is crucial in ensuring that patients receive the most effective and cost-efficient care possible. By requiring prior authorization, insurance companies can help prevent unnecessary treatments, reduce healthcare costs, and promote better health outcomes.
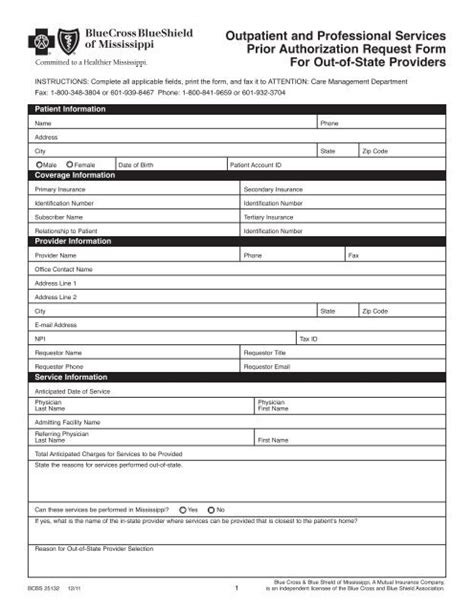
Blue Cross Blue Shield of Arizona Prior Auth Form
The Blue Cross Blue Shield of Arizona prior auth form is a specific document used by healthcare providers to request prior authorization for treatments, medications, or services for their patients. This form is typically completed by the healthcare provider and submitted to Blue Cross Blue Shield of Arizona for review.
Why is Prior Authorization Required?
Prior authorization is required for several reasons:
- To ensure medical necessity: Prior authorization helps ensure that treatments, medications, or services are medically necessary and align with the patient's diagnosis and treatment plan.
- To manage costs: Prior authorization helps manage healthcare costs by preventing unnecessary treatments and ensuring that patients receive the most cost-effective care possible.
- To promote quality care: Prior authorization promotes quality care by ensuring that patients receive evidence-based treatments and medications.
Steps Involved in the Prior Auth Process
The prior auth process involves several steps:
- Initial Request: The healthcare provider submits a prior auth request to Blue Cross Blue Shield of Arizona, typically through the online portal or by fax.
- Review: Blue Cross Blue Shield of Arizona reviews the request to determine whether the treatment, medication, or service is medically necessary and covered under the patient's insurance plan.
- Approval or Denial: Blue Cross Blue Shield of Arizona approves or denies the request, providing a written notification to the healthcare provider.
- Appeals: If the request is denied, the healthcare provider can appeal the decision by submitting additional information or documentation.

Benefits of Electronic Prior Auth
Electronic prior auth offers several benefits, including:
- Increased Efficiency: Electronic prior auth streamlines the process, reducing paperwork and increasing efficiency.
- Improved Accuracy: Electronic prior auth reduces errors, ensuring that requests are complete and accurate.
- Faster Turnaround Times: Electronic prior auth enables faster turnaround times, allowing healthcare providers to receive approval or denial notifications more quickly.
Tips for Submitting a Prior Auth Request
When submitting a prior auth request, healthcare providers should:
- Ensure completeness: Ensure that the request is complete and includes all required information and documentation.
- Use the correct form: Use the correct prior auth form, specific to Blue Cross Blue Shield of Arizona.
- Submit electronically: Submit the request electronically, whenever possible, to increase efficiency and reduce errors.
Common Prior Auth Forms
Blue Cross Blue Shield of Arizona offers various prior auth forms, including:
- Prior Auth Request Form: This form is used for general prior auth requests.
- Medication Prior Auth Form: This form is used specifically for medication prior auth requests.
- Durable Medical Equipment (DME) Prior Auth Form: This form is used specifically for DME prior auth requests.

Prior Auth Resources
Blue Cross Blue Shield of Arizona offers various resources to support healthcare providers with the prior auth process, including:
- Prior Auth Guidelines: Detailed guidelines outlining the prior auth process and requirements.
- Prior Auth Forms: Access to prior auth forms, including the prior auth request form, medication prior auth form, and DME prior auth form.
- Prior Auth FAQs: Frequently asked questions and answers related to the prior auth process.
Conclusion
In conclusion, the Blue Cross Blue Shield of Arizona prior auth form is a critical document used by healthcare providers to request prior authorization for treatments, medications, or services. Understanding the prior auth process, benefits, and tips for submitting a request can help healthcare providers navigate the process more efficiently. By leveraging electronic prior auth and utilizing available resources, healthcare providers can ensure that patients receive the necessary care while managing healthcare costs.
We encourage you to share your thoughts and experiences with the prior auth process in the comments below. Have you encountered any challenges or successes with prior authorization? Your input can help us better understand the complexities of the prior auth process and provide more effective support to healthcare providers.
What is prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a specific treatment, medication, or service is medically necessary and covered under a patient's insurance plan.
Why is prior authorization required?
+Prior authorization is required to ensure medical necessity, manage costs, and promote quality care.
How do I submit a prior auth request?
+You can submit a prior auth request through the online portal or by fax, using the correct prior auth form specific to Blue Cross Blue Shield of Arizona.