As a healthcare provider, navigating the complex world of insurance claims and appeals can be a daunting task. One of the most critical aspects of this process is mastering the BCBSM provider appeal form. In this article, we will guide you through the five easy steps to mastering the BCBSM provider appeal form, helping you to efficiently and effectively manage your appeals and get the reimbursement you deserve.
Healthcare providers deal with numerous administrative tasks, from patient care to insurance claims, and one of the most critical aspects is navigating the appeals process. The BCBSM provider appeal form is a crucial tool for providers to dispute denied claims and ensure fair reimbursement. However, the process can be overwhelming, especially for those new to the industry. By following these five easy steps, you can master the BCBSM provider appeal form and streamline your appeals process.

Step 1: Understand the BCBSM Appeal Process
Before diving into the provider appeal form, it's essential to understand the BCBSM appeal process. The process typically begins with a denied claim, followed by an initial appeal, and then a subsequent appeal to the Michigan Department of Insurance and Financial Services (DIFS). Understanding the different levels of appeal and the required documentation will help you prepare a stronger case.
- Initial Appeal: The provider submits an appeal to BCBSM, providing supporting documentation and explanations for the disputed claim.
- Reconsideration Appeal: If the initial appeal is denied, the provider can submit a reconsideration appeal to BCBSM, providing additional documentation and explanations.
- DIFS Appeal: If the reconsideration appeal is denied, the provider can submit an appeal to DIFS, which will review the case and make a final determination.
Key Takeaways:
- Understand the different levels of appeal and the required documentation.
- Familiarize yourself with the BCBSM appeal process and timelines.

Step 2: Gather Required Documentation
Gathering the required documentation is crucial to building a strong appeal case. The BCBSM provider appeal form requires specific information and documentation, including:
-
Claim denial letter
-
Patient demographics
-
Service dates and codes
-
Charged amount and payment information
-
Supporting medical records and documentation
-
Tips for gathering documentation:
- Ensure all documentation is accurate, complete, and legible.
- Organize documentation in a clear and concise manner.
- Include a cover letter explaining the appeal and providing context.
Key Takeaways:
- Gather all required documentation, including claim denial letters, patient demographics, and supporting medical records.
- Ensure documentation is accurate, complete, and legible.

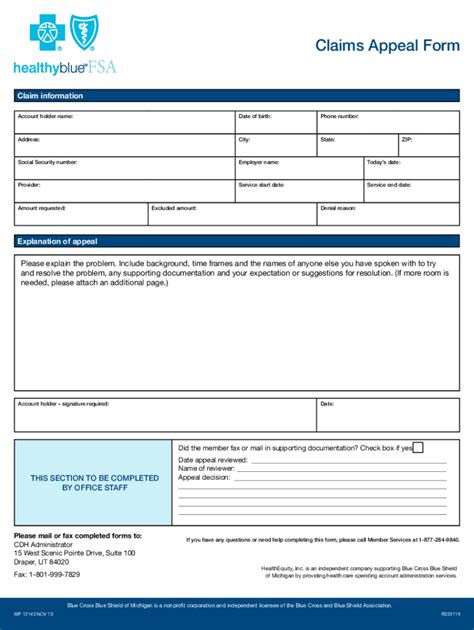
Step 3: Complete the BCBSM Provider Appeal Form
The BCBSM provider appeal form is a critical component of the appeal process. The form requires specific information, including:
-
Provider information
-
Patient demographics
-
Claim information
-
Appeal reason and explanation
-
Supporting documentation
-
Tips for completing the form:
- Ensure all information is accurate and complete.
- Use clear and concise language when explaining the appeal.
- Attach all supporting documentation.
Key Takeaways:
- Complete the BCBSM provider appeal form accurately and thoroughly.
- Use clear and concise language when explaining the appeal.

Step 4: Submit the Appeal
Once the appeal form is complete, it's time to submit the appeal to BCBSM. Ensure all documentation is included, and the form is signed and dated.
- Tips for submitting the appeal:
- Submit the appeal via fax, email, or mail, depending on BCBSM's requirements.
- Ensure the appeal is received by BCBSM within the required timeframe.
- Keep a copy of the appeal and documentation for your records.
Key Takeaways:
- Submit the appeal to BCBSM via the required method.
- Ensure the appeal is received within the required timeframe.

Step 5: Follow Up and Track the Appeal
After submitting the appeal, it's essential to follow up and track the status of the appeal. This can be done by contacting BCBSM directly or using their online portal.
- Tips for following up and tracking the appeal:
- Follow up with BCBSM within 7-10 business days to confirm receipt of the appeal.
- Use the online portal to track the status of the appeal.
- Keep a record of all communication with BCBSM.
Key Takeaways:
- Follow up with BCBSM to confirm receipt of the appeal.
- Use the online portal to track the status of the appeal.
By following these five easy steps, you can master the BCBSM provider appeal form and streamline your appeals process. Remember to stay organized, gather required documentation, and follow up with BCBSM to ensure a successful appeal.
Take the next step and share your experiences with the BCBSM provider appeal form in the comments below. How have you handled appeals in the past? What tips do you have for others? Share your thoughts and help us create a community of informed and empowered healthcare providers.
What is the BCBSM provider appeal form?
+The BCBSM provider appeal form is a document used by healthcare providers to dispute denied claims and request reimbursement from BCBSM.
What documentation is required for the BCBSM provider appeal form?
+The required documentation includes the claim denial letter, patient demographics, service dates and codes, charged amount and payment information, and supporting medical records and documentation.
How do I submit the BCBSM provider appeal form?
+The appeal form can be submitted via fax, email, or mail, depending on BCBSM's requirements. Ensure the appeal is received by BCBSM within the required timeframe.