Completing the BCBS TX Claim Review Form can seem like a daunting task, but it's actually a straightforward process that can be broken down into a few simple steps. In this article, we'll walk you through the process of completing the form, highlighting the importance of accuracy and attention to detail. Whether you're a healthcare provider, patient, or insurance representative, understanding the claim review process is crucial for smooth and efficient claim resolution.
Understanding the BCBS TX Claim Review Form

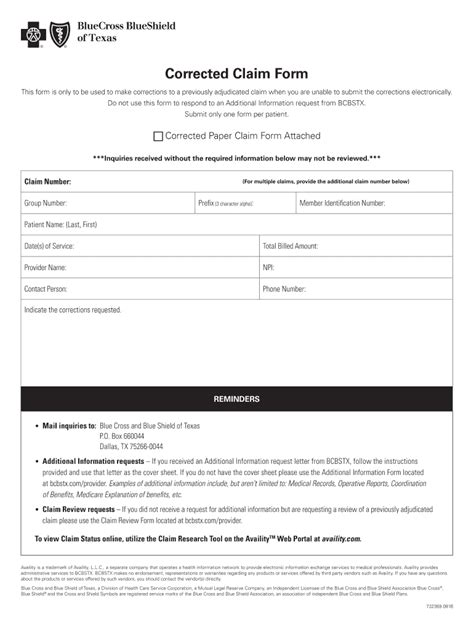
The BCBS TX Claim Review Form is a crucial document used by Blue Cross Blue Shield of Texas (BCBS TX) to review and process claims. The form is designed to gather essential information about the patient's treatment, medical history, and billing details. Accurate completion of the form is vital to ensure that claims are processed efficiently and accurately.
Why Accurate Completion Matters
Inaccurate or incomplete information on the claim review form can lead to delays, denials, or even claim rejection. This can result in additional administrative burdens, financial losses, and dissatisfaction for all parties involved. By following the steps outlined in this article, you can ensure that the claim review form is completed accurately and efficiently, minimizing the risk of errors and delays.
Step 1: Gather Required Information

Before starting the claim review form, make sure you have all the necessary information and documents. This includes:
- Patient demographics and insurance details
- Medical records and treatment information
- Billing and payment details
- Supporting documentation, such as lab results or medical images
Having all the required information readily available will save time and reduce the risk of errors.
What to Include
When gathering information, make sure to include the following:
- Patient name, date of birth, and insurance ID number
- Diagnosis and treatment codes
- Dates of service and billing information
- Supporting documentation, such as lab results or medical images
Step 2: Complete Patient Information Section

The patient information section is a critical part of the claim review form. Ensure that you accurately complete the following fields:
- Patient name and date of birth
- Insurance ID number and group number
- Address and contact information
Double-check the patient's demographics to ensure accuracy and consistency with their insurance records.
Tips for Accuracy
- Verify patient demographics against their insurance card or records
- Use the patient's full name and date of birth to avoid confusion
- Ensure the insurance ID number and group number are accurate and up-to-date
Step 3: Complete Medical Information Section

The medical information section requires detailed information about the patient's treatment and medical history. Ensure that you accurately complete the following fields:
- Diagnosis and treatment codes
- Dates of service and procedure codes
- Supporting documentation, such as lab results or medical images
Use clear and concise language when describing the patient's medical condition and treatment.
What to Include
When completing the medical information section, make sure to include:
- Accurate diagnosis and treatment codes
- Detailed descriptions of procedures and services
- Supporting documentation, such as lab results or medical images
Step 4: Complete Billing and Payment Information Section

The billing and payment information section requires accurate completion of billing and payment details. Ensure that you accurately complete the following fields:
- Billing information, including provider name and address
- Payment information, including amount and payment method
- Supporting documentation, such as invoices or payment receipts
Use clear and concise language when describing billing and payment details.
Tips for Accuracy
- Verify billing and payment information against invoices and payment records
- Use clear and concise language when describing billing and payment details
- Ensure supporting documentation is accurate and up-to-date
Step 5: Review and Submit the Claim Review Form

Once you've completed the claim review form, review it carefully for accuracy and completeness. Ensure that all required fields are completed and supporting documentation is attached.
Submit the claim review form to BCBS TX, either electronically or by mail, depending on the preferred submission method.
Tips for Submission
- Review the claim review form carefully for accuracy and completeness
- Ensure all required fields are completed and supporting documentation is attached
- Submit the claim review form promptly to avoid delays
By following these 5 easy steps, you can ensure that the BCBS TX Claim Review Form is completed accurately and efficiently, minimizing the risk of errors and delays.
Now that you've completed the claim review form, take a moment to review and verify the information. If you have any questions or concerns, don't hesitate to reach out to BCBS TX for assistance.
We invite you to share your thoughts and experiences with completing the BCBS TX Claim Review Form in the comments below. Your feedback and insights can help others navigate the claim review process more efficiently.
What is the BCBS TX Claim Review Form used for?
+The BCBS TX Claim Review Form is used by Blue Cross Blue Shield of Texas (BCBS TX) to review and process claims. The form gathers essential information about the patient's treatment, medical history, and billing details.
How do I ensure accurate completion of the claim review form?
+To ensure accurate completion of the claim review form, gather all required information and documents, verify patient demographics and billing information, and use clear and concise language when describing medical and billing details.
What happens if I make an error on the claim review form?
+If you make an error on the claim review form, it can lead to delays, denials, or even claim rejection. Review the form carefully for accuracy and completeness before submission, and correct any errors promptly.