Navigating the complex world of Medicare Advantage plans can be overwhelming, especially when it comes to prior authorization. As a healthcare provider or patient, understanding the requirements and process for prior authorization is crucial to ensure smooth and efficient care. In this article, we will delve into the specifics of BCBS Medicare Advantage prior authorization form requirements, exploring the ins and outs of this critical process.

Why is Prior Authorization Important?
Prior authorization is a critical step in the healthcare process, ensuring that patients receive medically necessary treatments and services while minimizing unnecessary costs. By requiring prior authorization, BCBS Medicare Advantage plans can:
- Verify the medical necessity of treatments and services
- Prevent unnecessary or duplicate procedures
- Ensure that patients receive the most effective and efficient care
- Manage healthcare costs and minimize waste
BCBS Medicare Advantage Prior Authorization Form Requirements
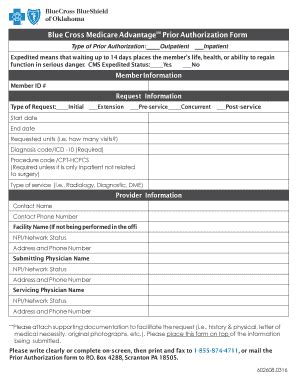
To initiate the prior authorization process, healthcare providers must submit a completed prior authorization form to BCBS. The form requirements may vary depending on the specific plan and service or treatment being requested. However, here are some general requirements:
- Patient Information: The form must include the patient's name, date of birth, and Medicare Advantage plan ID number.
- Service or Treatment Information: A clear description of the service or treatment being requested, including the CPT or HCPCS code, must be provided.
- Medical Necessity: A statement explaining the medical necessity of the service or treatment, including any relevant medical history or diagnosis.
- Provider Information: The healthcare provider's name, address, and contact information must be included.
- Supporting Documentation: Additional documentation, such as medical records or test results, may be required to support the prior authorization request.
Types of Prior Authorization Forms
BCBS Medicare Advantage plans use different prior authorization forms for various services and treatments. Some common types of forms include:
- Standard Prior Authorization Form: Used for most services and treatments, including doctor visits, tests, and procedures.
- Durable Medical Equipment (DME) Prior Authorization Form: Used for DME requests, such as wheelchairs, oxygen therapy, or hospital beds.
- Pharmacy Prior Authorization Form: Used for prescription medication requests.
Submission and Review Process
Once the prior authorization form is completed, it must be submitted to BCBS for review. The submission process typically involves:
- Fax or Mail: Forms can be faxed or mailed to the designated BCBS prior authorization department.
- Online Portal: Some BCBS plans offer online portals for electronic submission and tracking of prior authorization requests.
- Review: BCBS reviews the submitted form and supporting documentation to determine medical necessity and coverage.
Prior Authorization Timeframes and Response
The timeframe for prior authorization review and response varies depending on the BCBS plan and the type of service or treatment being requested. However, here are some general guidelines:
- Standard Prior Authorization: 3-5 business days for review and response
- Expedited Prior Authorization: 24-48 hours for review and response (for urgent or emergency situations)
- DME Prior Authorization: 5-10 business days for review and response
Tips for Streamlining the Prior Authorization Process
To minimize delays and ensure a smooth prior authorization process, healthcare providers can:
- Verify Patient Eligibility: Confirm patient eligibility and coverage before submitting a prior authorization request.
- Use Correct Forms: Ensure the correct prior authorization form is used for the specific service or treatment being requested.
- Submit Complete Information: Provide complete and accurate information, including supporting documentation, to avoid delays or denials.
- Follow Up: Follow up with BCBS to confirm receipt of the prior authorization request and to inquire about the status of the review.

Common Reasons for Prior Authorization Denials
Prior authorization requests can be denied for various reasons, including:
- Lack of Medical Necessity: The requested service or treatment is not deemed medically necessary.
- Incomplete or Inaccurate Information: The prior authorization form or supporting documentation is incomplete or inaccurate.
- Non-Covered Service: The requested service or treatment is not covered under the BCBS Medicare Advantage plan.
Appealing a Prior Authorization Denial
If a prior authorization request is denied, healthcare providers can appeal the decision by:
- Submitting Additional Information: Providing additional documentation or information to support the prior authorization request.
- Requesting a Re-Review: Requesting a re-review of the prior authorization request.
- Escalating the Appeal: Escalating the appeal to a higher level of review, such as a peer-to-peer review or an external review.
Conclusion and Next Steps
In conclusion, understanding the BCBS Medicare Advantage prior authorization form requirements is essential for healthcare providers and patients. By following the guidelines and tips outlined in this article, providers can streamline the prior authorization process, minimize delays, and ensure that patients receive the necessary care and services.
If you have any questions or concerns about the prior authorization process or would like to share your experiences, please comment below. Don't forget to share this article with your colleagues and patients to help them navigate the complex world of Medicare Advantage prior authorization.
What is prior authorization, and why is it required?
+Prior authorization is a process that requires healthcare providers to obtain approval from the insurance company before providing certain services or treatments. It is required to ensure that patients receive medically necessary care and to manage healthcare costs.
What information is required on a BCBS Medicare Advantage prior authorization form?
+The prior authorization form requires patient information, service or treatment information, medical necessity statement, provider information, and supporting documentation.
How long does the prior authorization review process take?
+The review process typically takes 3-5 business days for standard prior authorization requests, 24-48 hours for expedited requests, and 5-10 business days for DME prior authorization requests.