What is Amerigroup Prior Authorization Form and Why is it Important?

Prior authorization is a crucial step in the healthcare process that ensures patients receive necessary treatments and medications while also controlling healthcare costs. Amerigroup, a leading healthcare provider, requires prior authorization for certain medical services and prescriptions to ensure that patients receive the most effective and cost-efficient care possible. The Amerigroup Prior Authorization Form is a crucial document that healthcare providers must complete to obtain approval for these services.
The Benefits of Prior Authorization
Prior authorization offers several benefits, including:
- Ensures patients receive necessary treatments and medications
- Helps control healthcare costs by reducing unnecessary procedures and prescriptions
- Promotes communication between healthcare providers and payers
- Streamlines the healthcare process, reducing delays and denials
Step 1: Determine if Prior Authorization is Required

Before starting the prior authorization process, healthcare providers must determine if prior authorization is required for the specific medical service or prescription. Amerigroup provides a list of services and medications that require prior authorization on their website. Healthcare providers can also contact Amerigroup's customer service department to determine if prior authorization is required.
Services that Typically Require Prior Authorization
- Certain prescription medications
- Surgical procedures
- Diagnostic tests (e.g., MRI, CT scans)
- Durable medical equipment (e.g., wheelchairs, oxygen tanks)
Step 2: Gather Required Information and Documents

To complete the prior authorization process, healthcare providers must gather the required information and documents. This may include:
- Patient's medical history and diagnosis
- Proposed treatment plan
- Prescription medication information (if applicable)
- Results of diagnostic tests (if applicable)
Additional Information that May be Required
- Patient's medical records
- Laboratory results
- Imaging studies (e.g., X-rays, MRI)
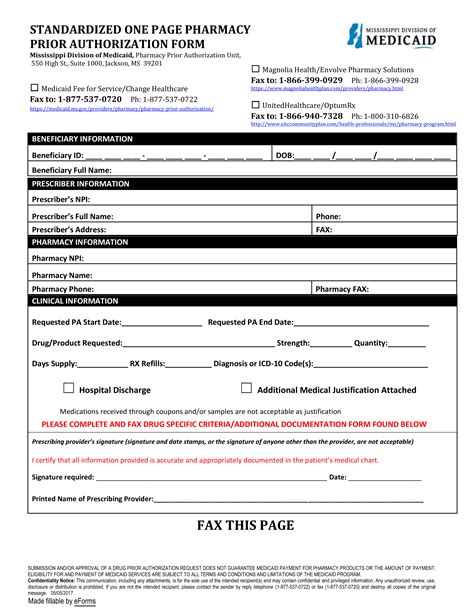
Step 3: Complete the Amerigroup Prior Authorization Form

Once the required information and documents are gathered, healthcare providers can complete the Amerigroup Prior Authorization Form. The form can be downloaded from Amerigroup's website or obtained by contacting their customer service department. The form must be completed in its entirety and include all required information and documentation.
Information to Include on the Form
- Patient's demographic information
- Medical diagnosis and proposed treatment plan
- Prescription medication information (if applicable)
- Results of diagnostic tests (if applicable)
Step 4: Submit the Prior Authorization Request

Once the prior authorization form is complete, healthcare providers can submit the request to Amerigroup. The request can be submitted via fax, email, or online through Amerigroup's website. Healthcare providers should ensure that the request is submitted with all required information and documentation to avoid delays or denials.
Submission Methods
- Fax: [insert fax number]
- Email: [insert email address]
- Online: [insert website URL]
Step 5: Receive and Review the Prior Authorization Decision

After submitting the prior authorization request, healthcare providers will receive a decision from Amerigroup. The decision will be based on the medical necessity of the requested service or medication. If approved, the patient can proceed with the treatment or receive the prescribed medication. If denied, the healthcare provider can appeal the decision or submit additional information to support the request.
What to Do if the Request is Denied
- Review the denial letter and ensure that all required information and documentation were submitted
- Submit an appeal with additional information or documentation to support the request
- Contact Amerigroup's customer service department for assistance
By following these 5 easy steps, healthcare providers can ensure a smooth prior authorization process and obtain the necessary approvals for their patients to receive the medical services and prescriptions they need.
Take Action Today

Don't let prior authorization hold you back from providing the best possible care for your patients. By understanding the prior authorization process and following these 5 easy steps, you can ensure that your patients receive the medical services and prescriptions they need in a timely and efficient manner. Contact Amerigroup today to learn more about their prior authorization process and to obtain the necessary forms and documentation.
We encourage you to share your thoughts and experiences with the prior authorization process in the comments section below. Your feedback can help us improve the process and provide better care for our patients.
FAQ Section:
What is prior authorization?
+Prior authorization is a process that requires healthcare providers to obtain approval from a payer before providing certain medical services or prescribing certain medications.
Why is prior authorization required?
+Prior authorization is required to ensure that patients receive necessary treatments and medications while also controlling healthcare costs.
How long does the prior authorization process take?
+The prior authorization process typically takes a few days to a few weeks, depending on the complexity of the request and the payer's processing time.