Prior authorization, also known as pre-authorization, is a crucial step in the healthcare process that ensures patients receive necessary treatments while minimizing costs. For healthcare providers and patients enrolled in Ambetter health insurance plans, navigating the prior authorization process can be overwhelming. In this article, we will delve into the Ambetter prior authorization form, providing a step-by-step guide to help you understand the process and streamline your workflow.
The importance of prior authorization cannot be overstated. By verifying the medical necessity of treatments, prior authorization helps prevent unnecessary costs, reduces waste, and ensures that patients receive evidence-based care. For healthcare providers, prior authorization is a critical component of ensuring compliance with regulatory requirements and maintaining a smooth billing process.

Understanding the Ambetter Prior Authorization Process
Before we dive into the step-by-step guide, it's essential to understand the Ambetter prior authorization process. Ambetter is a health insurance marketplace plan that offers a range of coverage options for individuals and families. As part of their commitment to providing high-quality, affordable care, Ambetter requires prior authorization for certain treatments, medications, and services.
Ambetter's prior authorization process involves a thorough review of the patient's medical history, current treatment plan, and the requested service or medication. This review is typically conducted by a team of healthcare professionals who assess the medical necessity of the requested service or medication.
Benefits of Prior Authorization
Prior authorization offers several benefits for patients, healthcare providers, and payers:
- Improved patient outcomes: By ensuring that patients receive evidence-based care, prior authorization helps improve treatment outcomes and reduces the risk of adverse events.
- Reduced costs: Prior authorization helps minimize unnecessary costs by verifying the medical necessity of treatments and preventing overutilization.
- Streamlined workflow: Prior authorization can help reduce administrative burdens on healthcare providers by automating the approval process and minimizing paperwork.

A Step-By-Step Guide to the Ambetter Prior Authorization Form
Now that we've covered the importance of prior authorization and the benefits it offers, let's dive into the step-by-step guide to the Ambetter prior authorization form.
Step 1: Determine if Prior Authorization is Required
Before submitting a prior authorization request, healthcare providers must determine if the service or medication requires prior authorization. Ambetter provides a list of services and medications that require prior authorization on their website.
Step 2: Gather Required Information
To complete the prior authorization form, healthcare providers will need to gather the following information:
- Patient demographics and insurance information
- Medical history and current treatment plan
- Requested service or medication, including dosage and frequency
- Clinical rationale for the requested service or medication

Step 3: Complete the Prior Authorization Form
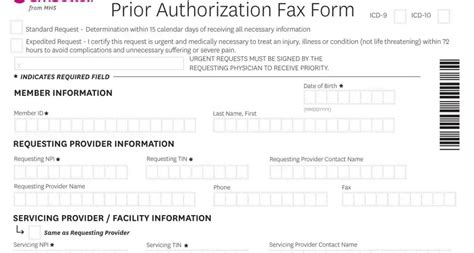
The Ambetter prior authorization form is typically completed by the healthcare provider or their staff. The form requires the following information:
- Patient information, including name, date of birth, and insurance ID number
- Requested service or medication, including dosage and frequency
- Clinical rationale for the requested service or medication
- Supporting documentation, such as medical records and test results
Step 4: Submit the Prior Authorization Request
Once the prior authorization form is complete, healthcare providers can submit the request to Ambetter via fax, email, or online portal.
Step 5: Review and Response
Ambetter's prior authorization team will review the request and respond with a determination. If approved, the patient can proceed with the requested service or medication. If denied, the healthcare provider can appeal the decision or provide additional information to support the request.

Additional Tips and Considerations
- Ensure accurate and complete information: Incomplete or inaccurate information can delay the prior authorization process. Ensure that all required fields are complete and accurate.
- Submit supporting documentation: Supporting documentation, such as medical records and test results, can help support the prior authorization request.
- Follow up with Ambetter: If you haven't received a response from Ambetter within a few days, follow up with their customer service team to ensure that your request is being processed.

Conclusion
In conclusion, the Ambetter prior authorization form is a critical component of ensuring that patients receive necessary treatments while minimizing costs. By understanding the prior authorization process and following the step-by-step guide, healthcare providers can streamline their workflow and reduce administrative burdens.
We hope that this article has provided valuable insights into the Ambetter prior authorization form and process. If you have any questions or comments, please don't hesitate to share them with us.

What is prior authorization?
+Prior authorization is a process that verifies the medical necessity of a treatment, medication, or service before it is provided to a patient.
How do I determine if prior authorization is required?
+Ambetter provides a list of services and medications that require prior authorization on their website. You can also contact their customer service team to determine if prior authorization is required.
How long does the prior authorization process take?
+The prior authorization process typically takes a few days to a week, depending on the complexity of the request and the availability of supporting documentation.