Prior authorization (PA) is a crucial step in the healthcare process, ensuring that patients receive the necessary treatments while minimizing unnecessary costs. For healthcare providers, managing PA requirements can be time-consuming and complex. One of the most commonly used prior authorization forms is the Aim Specialty Prior Authorization Form. In this article, we will provide you with 5 valuable tips to help you complete this form efficiently and effectively.
Understanding the Aim Specialty Prior Authorization Form
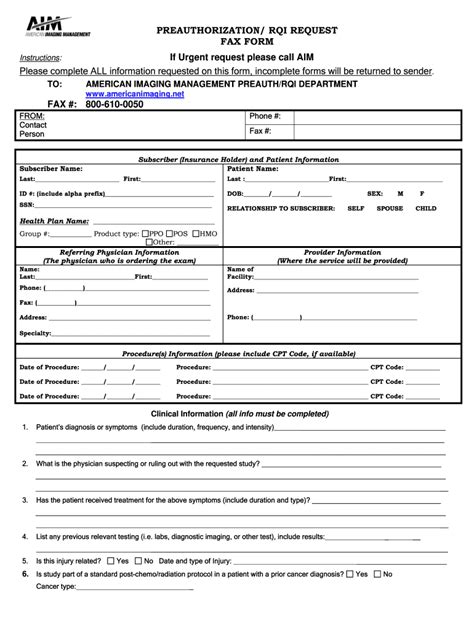
The Aim Specialty Prior Authorization Form is a document required by Anthem, Inc. (a leading health insurance company) to review and approve prior authorization requests for specialty medications and treatments. The form is designed to gather essential information about the patient's condition, treatment plan, and medication regimen, allowing Anthem to make informed decisions about coverage.
Tip 1: Gather All Necessary Information Before Starting
To complete the Aim Specialty Prior Authorization Form efficiently, it's essential to gather all necessary information before starting. This includes:
- Patient demographics and medical history
- Current treatment plan and medication regimen
- Relevant medical records and test results
- Information about the requested medication or treatment

Having all the necessary information readily available will save you time and reduce the risk of errors or omissions.
Tip 2: Use Clear and Concise Language
When completing the Aim Specialty Prior Authorization Form, it's crucial to use clear and concise language. Avoid using abbreviations or medical jargon that may be unfamiliar to non-medical reviewers. Instead, use simple and straightforward language to describe the patient's condition, treatment plan, and medication regimen.
Tip 3: Provide Detailed Rationale for Treatment
The Aim Specialty Prior Authorization Form requires a detailed rationale for the requested treatment or medication. This section is critical, as it helps Anthem reviewers understand the clinical justification for the treatment plan. When completing this section, be sure to:
- Clearly explain the patient's condition and how it meets the coverage criteria
- Provide evidence-based information supporting the treatment plan
- Address any potential concerns or questions Anthem reviewers may have
Tip 4: Attach Supporting Documentation
To support the prior authorization request, it's essential to attach relevant supporting documentation, such as:
- Medical records and test results
- Treatment plans and medication regimens
- Letters of medical necessity

Make sure to carefully review the form instructions to ensure you're attaching the required documentation.
Tip 5: Review and Verify Information Before Submitting
Before submitting the Aim Specialty Prior Authorization Form, it's crucial to review and verify all information for accuracy and completeness. Double-check the patient's demographics, medical history, and treatment plan to ensure everything is correct.

A careful review will help minimize errors and reduce the risk of delays or denials.
Streamlining the Prior Authorization Process
By following these 5 tips, you can streamline the prior authorization process and increase the likelihood of approval. Remember to:
- Gather all necessary information before starting
- Use clear and concise language
- Provide detailed rationale for treatment
- Attach supporting documentation
- Review and verify information before submitting
By taking the time to carefully complete the Aim Specialty Prior Authorization Form, you can help ensure that your patients receive the necessary treatments while minimizing unnecessary delays or denials.
Take Action!
Have you found this article helpful? Share your experiences with prior authorization and how you've streamlined the process. Do you have any questions or concerns about the Aim Specialty Prior Authorization Form? Leave a comment below, and we'll do our best to address your queries.
Frequently Asked Questions
What is the Aim Specialty Prior Authorization Form?
+The Aim Specialty Prior Authorization Form is a document required by Anthem, Inc. to review and approve prior authorization requests for specialty medications and treatments.
What information do I need to gather before starting the form?
+You'll need to gather patient demographics, medical history, current treatment plan, and medication regimen, as well as relevant medical records and test results.
How long does it take to complete the Aim Specialty Prior Authorization Form?
+The time it takes to complete the form will vary depending on the complexity of the case and the amount of information required. On average, it can take 30 minutes to an hour to complete the form.