Understanding Aetna's Prior Authorization Process for Prolia

For patients suffering from osteoporosis, Prolia (denosumab) is a crucial medication that helps prevent bone fractures. However, obtaining approval for this medication can be a daunting task, especially when dealing with insurance providers like Aetna. In this article, we will delve into the world of prior authorization, focusing on Aetna's process for Prolia, and provide a comprehensive guide to help you navigate this complex system.
The Importance of Prior Authorization
Prior authorization is a process used by insurance providers to ensure that medications are prescribed and used responsibly. This process helps prevent unnecessary or excessive use of medications, reducing healthcare costs and potential side effects. For patients, prior authorization can be a source of frustration, as it often involves lengthy paperwork and waiting periods. However, understanding the process and requirements can make a significant difference in obtaining the necessary medication.
Aetna's Prior Authorization Process for Prolia

Aetna's prior authorization process for Prolia involves several steps:
- Patient Eligibility: The patient must be a member of Aetna's insurance plan, and the medication must be included in their coverage.
- Prescription and Medical Records: The patient's healthcare provider must submit a prescription for Prolia, along with relevant medical records, to Aetna's prior authorization department.
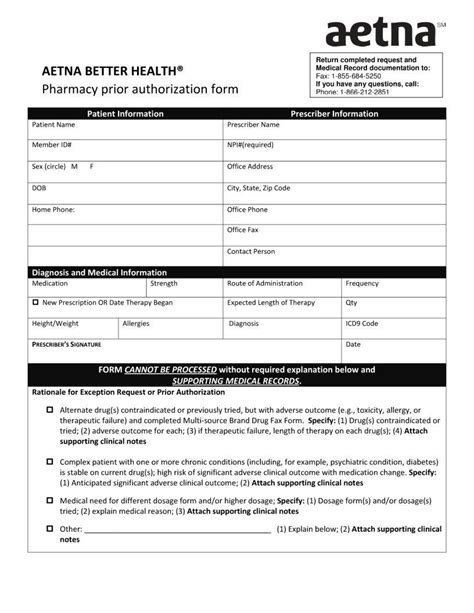
- Prior Authorization Form: Aetna will provide a prior authorization form, which the healthcare provider must complete and return. This form requires detailed information about the patient's medical condition, treatment history, and medication regimen.
- Review and Approval: Aetna's prior authorization team will review the submitted information and make a determination regarding coverage.
Required Documents for Prior Authorization
To ensure a smooth prior authorization process, the following documents are typically required:
- Prolia Prior Authorization Form: Aetna's standardized form, which must be completed by the healthcare provider.
- Prescription: A valid prescription for Prolia, written by the patient's healthcare provider.
- Medical Records: Relevant medical records, including test results, diagnoses, and treatment plans.
- Lab Results: Laboratory results, such as bone density tests, to support the diagnosis of osteoporosis.
Completing the Aetna Prolia Prior Authorization Form

The Aetna Prolia prior authorization form requires detailed information about the patient's medical condition, treatment history, and medication regimen. To ensure accuracy and completeness, follow these steps:
- Section 1: Patient Information: Enter the patient's demographic information, including name, date of birth, and insurance ID number.
- Section 2: Medical Information: Provide detailed information about the patient's medical condition, including diagnosis, treatment history, and relevant test results.
- Section 3: Medication Information: List all medications the patient is currently taking, including dosages and frequencies.
- Section 4: Prolia-Specific Information: Answer questions specific to Prolia, such as the patient's bone density test results and treatment goals.
Tips for a Successful Prior Authorization
To increase the chances of a successful prior authorization, keep the following tips in mind:
- Submit Complete and Accurate Information: Ensure that all required documents are submitted, and the prior authorization form is completed accurately.
- Provide Supporting Documentation: Include relevant medical records, lab results, and test results to support the patient's diagnosis and treatment plan.
- Follow Aetna's Guidelines: Adhere to Aetna's prior authorization process and guidelines to avoid delays or denials.
What to Expect After Submitting the Prior Authorization Form

After submitting the prior authorization form, Aetna's prior authorization team will review the information and make a determination regarding coverage. This process typically takes several days to several weeks.
- Approval: If the prior authorization is approved, Aetna will notify the patient's healthcare provider, and the medication will be covered.
- Denial: If the prior authorization is denied, Aetna will provide a written explanation for the denial, and the patient's healthcare provider can appeal the decision.
- Additional Information Requested: If Aetna requires additional information, the patient's healthcare provider will be notified, and the prior authorization process will be delayed until the requested information is received.
Conclusion
Navigating Aetna's prior authorization process for Prolia can be challenging, but understanding the requirements and guidelines can make a significant difference in obtaining the necessary medication. By following the steps outlined in this guide, patients and healthcare providers can increase the chances of a successful prior authorization and ensure that patients receive the medication they need to manage osteoporosis.
What is the Aetna Prolia prior authorization form?
+The Aetna Prolia prior authorization form is a document required by Aetna to evaluate the medical necessity of Prolia for patients with osteoporosis.
What documents are required for the Aetna Prolia prior authorization process?
+The required documents include the Prolia prior authorization form, prescription, medical records, and lab results.
How long does the Aetna Prolia prior authorization process take?
+The prior authorization process typically takes several days to several weeks.