Aetna Medicare viscosupplementation approval can be a lengthy and complex process, but with the right guidance, you can navigate it successfully. Viscosupplementation is a non-surgical treatment for osteoarthritis that involves injecting hyaluronic acid into the affected joint to reduce pain and inflammation. Aetna Medicare provides coverage for this treatment, but prior authorization is required. Here's a step-by-step guide to help you obtain approval:
Getting to Know Viscosupplementation and Its Benefits
Viscosupplementation is a popular treatment for osteoarthritis, particularly for patients who have not responded well to other treatments. It involves injecting hyaluronic acid, a naturally occurring substance in the body, into the affected joint to reduce pain and inflammation. The benefits of viscosupplementation include:
- Reduced pain and inflammation
- Improved joint mobility
- Delayed need for surgery
- Minimally invasive procedure
However, to receive coverage from Aetna Medicare, you need to meet specific criteria and follow the necessary steps.
Step 1: Meet the Eligibility Criteria

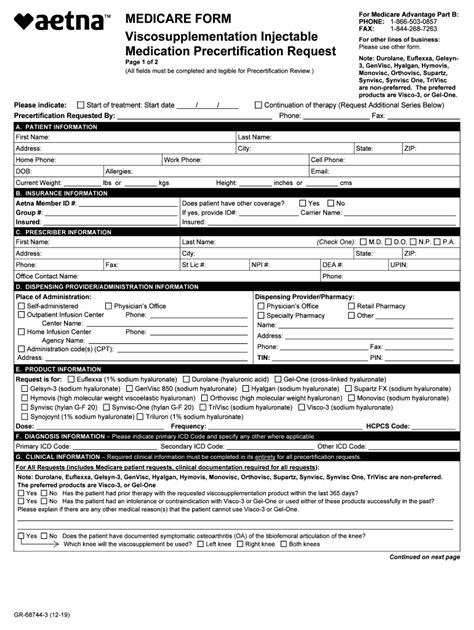
To qualify for Aetna Medicare viscosupplementation approval, you must meet the following criteria:
- Be diagnosed with osteoarthritis of the knee or other joints
- Have failed to respond to other treatments, such as physical therapy, pain medication, or corticosteroid injections
- Be a candidate for joint replacement surgery
- Have not had viscosupplementation treatment in the past 6 months
Your healthcare provider will assess your condition and determine if you meet the eligibility criteria.
Additional Requirements
In addition to meeting the eligibility criteria, you may need to provide additional documentation, such as:
- Medical records and test results
- X-rays or MRI scans
- Documentation of previous treatments and their outcomes
Your healthcare provider will guide you through the process and ensure that all necessary documentation is submitted.
Step 2: Choose an Approved Viscosupplementation Product

Aetna Medicare has approved several viscosupplementation products, including:
- Hyalgan
- Synvisc
- Euflexxa
- Orthovisc
Your healthcare provider will recommend an approved product based on your specific needs and medical condition.
Product-Specific Requirements
Each approved product has its own set of requirements and guidelines. For example, some products may require a specific dosage or administration schedule. Your healthcare provider will ensure that all product-specific requirements are met.
Step 3: Submit a Prior Authorization Request

Once you have met the eligibility criteria and chosen an approved product, your healthcare provider will submit a prior authorization request to Aetna Medicare. This request will include:
- Your medical history and diagnosis
- Documentation of previous treatments and their outcomes
- The recommended viscosupplementation product and dosage
Aetna Medicare Review Process
Aetna Medicare will review your prior authorization request and may request additional information or documentation. This process can take several days to several weeks, depending on the complexity of your case.
Step 4: Receive Approval and Schedule Treatment

If your prior authorization request is approved, your healthcare provider will schedule the viscosupplementation treatment. This may involve a series of injections, typically 3-5 injections, spaced 1-2 weeks apart.
Treatment Administration
The viscosupplementation treatment will be administered by a healthcare professional in a clinical setting. You may experience some discomfort or pain during the injection, but this is usually temporary.
Step 5: Follow-Up and Monitoring

After the treatment, your healthcare provider will monitor your progress and adjust your treatment plan as needed. This may involve follow-up appointments and additional treatments.
Outcome Assessment
Your healthcare provider will assess the outcome of the treatment and determine if additional treatments are necessary. This may involve evaluating your pain levels, joint mobility, and overall quality of life.
Conclusion and Call to Action
Obtaining Aetna Medicare viscosupplementation approval requires careful planning and attention to detail. By following these steps and working closely with your healthcare provider, you can navigate the process successfully and receive the treatment you need. If you have any questions or concerns, don't hesitate to reach out to your healthcare provider or Aetna Medicare.
Share your experiences with viscosupplementation and Aetna Medicare approval in the comments below. Have you had success with this treatment? What challenges did you face during the approval process?
What is viscosupplementation?
+Viscosupplementation is a non-surgical treatment for osteoarthritis that involves injecting hyaluronic acid into the affected joint to reduce pain and inflammation.
What are the benefits of viscosupplementation?
+The benefits of viscosupplementation include reduced pain and inflammation, improved joint mobility, delayed need for surgery, and a minimally invasive procedure.
How do I qualify for Aetna Medicare viscosupplementation approval?
+To qualify for Aetna Medicare viscosupplementation approval, you must meet specific criteria, including a diagnosis of osteoarthritis, failure to respond to other treatments, and being a candidate for joint replacement surgery.